The Rise and Impending Fall of the Dental Cavity
Another of history's great killers is on the chopping block
You Have Your Mother’s Cavities
Cavities are a communicable disease, and if you’re among the 90% of Americans who’s ever had one, you probably got them from your mother.1
This isn’t to say that you were directly infected with cavities by your mother, but that due to the everyday interactions where parents end up exchanging spit with their children, at some point, your oral microbiome probably came to resemble hers. You share food, you share drinks, you share utensils and silverware, and as a result, your clean infant mouth was eventually colonized by your mother’s strain of the main cavity-causing bacteria Streptococcus mutans.2
After S. mutans has taken up residence in your gluttonous abode, that’s when the magic happens.
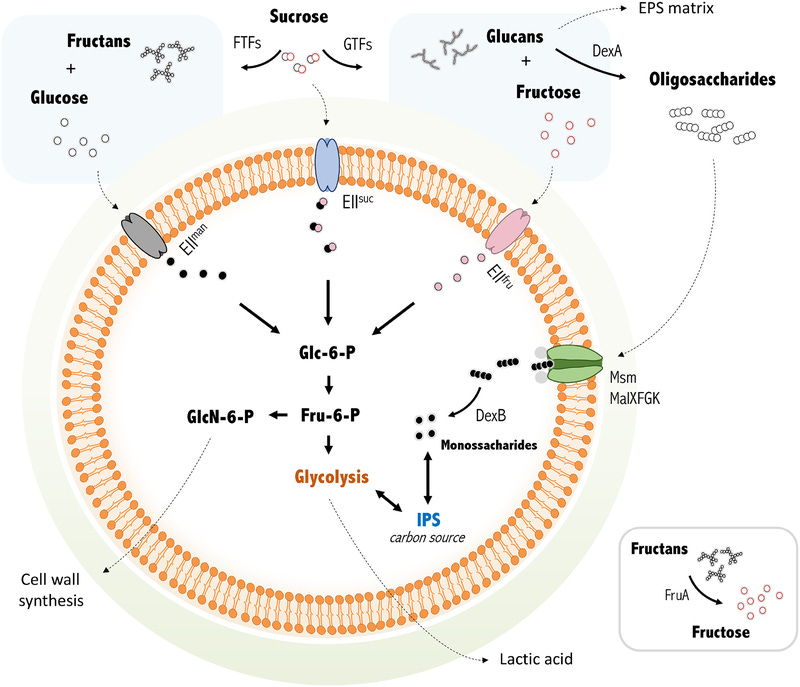
S. mutans is a carbaholic—it absolutely loves carbs. The primary way it gets its energy is through using the magic of glycolysis to break down sugar, bread, and everything else it can touch, producing several acidic byproducts in the process. The main organic acid produced as a result of S. mutans’ feeding is lactic acid.
With lactic acid in your mouth, the pH falls, leaving your mouth more acidic and hostile to its mineral inhabits—your teeth. The acidified environment begins to demineralize tooth enamel, making it rough, causing pits to form and widen. When those pits are large enough, that’s a cavity.
This process has been shown experimentally in vivid detail. In the journal Dental Materials, Cross et al. presented profilometry images of what happens to teeth after exposure to a 30% lactic acid solution. The result of doing this is shown in images a, b, c, and d, below, which are, respectively, polished enamel and the same enamel after 45, 90, and 225 minutes. It clearly becomes much less smooth and vastly more rough as time in the acid continues. You’ll also notice images e and f, which are, respectively, another clean enamel surface and the same surface after 72 hours of colonization by S. mutans.3
Acidic environments rip through teeth, and the other bacteria living in the mouth are generally happy to take advantage of this situation, often making things worse.4
The Revolutionary Origins of Dental Decay
We know how people get the bacteria that drives the formation of dental cavities (henceforth “caries”), and we know how they work, but how long have animals had to deal with dental decay?
There are currently no publications documenting caries in dinosaurs. We have plenty of records indicating mechanical wear and tear, but none showing that dinosaurs were beset by caries. This might be shocking since some of the toothiest dinosaurs had extraordinarily thin enamel, so it wouldn’t take much for caries to form. But even today, many animals renowned for their smiles don’t seem to get caries despite thin enamel—the alligator is a familiar example.
The standard explanation for the co-occurrence of thin enamel and absent caries is that the relevant animals are polyphyodonts,5 meaning that their teeth are continually replaced over the lifespan. But this explanation isn’t that great unless you believe that teeth are dropped as soon as decay sets in, and that’s not realistic. More likely, the reason caries are so rare among so many animals is because their diets aren’t usually sugar-rich, and there’s just not much for S. mutans to ferment even if the bacteria has taken up residence in their mouths.6
S. mutans has a special affinity for sucrose—table sugar—, a disaccharide combination of glucose and fructose. While there are few animals whose diets are rich in sucrose, there are plenty of frugivorous animals who have fructose-rich diets. The fact that the first true fruits made their appearance in the late Cretaceous might go a long way to explaining why there are so few known frugivorous dinosaurs7 and why caries haven’t yet been documented among them. I think this case is further strengthened by the finding that dinosaur teeth often contained fluorapatite instead of hydroxyapatite like our teeth. That means that if those dinosaur’s diets were conducive to S. mutans or were otherwise acidifying, their teeth would have been noticeably melted; not only that, the melting would have produced hydrogen fluoride, killing dinosaurs unless they had some never-before-observed means of resisting it.8
So we’ll have to start the story of caries a little later than the dinosaurs.
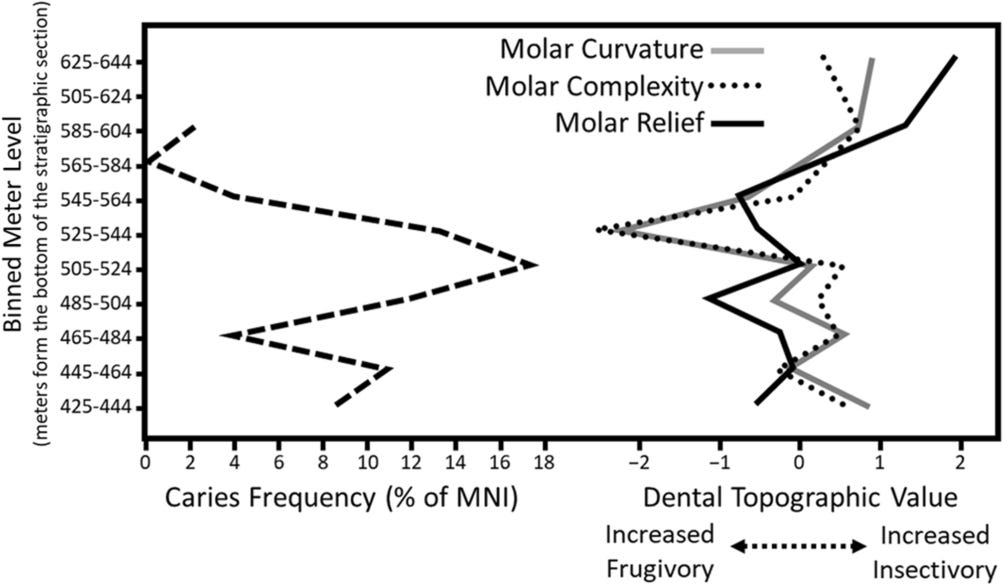
The earliest-known example of caries in a mammal was published in 2021. Microsyops latidens was a stem primate found in Wyoming. This proto-monkey existed for about 500,000 years before going extinct 54 million years ago, so the samples are old.
1,030 Microsyops specimens were uncovered and 7.5% of them had caries, but the proportion of individuals with caries varied considerably over time. In the time period caries were most frequent, every sixth Microsyops specimen had them. Because we also have knowledge about their diets throughout the sampling period, this excess of caries can be used to affirm what I said above: diet matters. The period with the greatest frequency of caries seemed to be the one with the greatest levels of fruit consumption and thus the dietary environment most conducive to acidification.9
Ancient monkeys don’t have anything on modern humans. The CDC reports that 9/10 Americans have had caries before. Moreover, a quarter of the U.S. population was estimated to have untreated dental decay. That’s a lot of decay, and it’s not unique to America either. The 2019 Global Burden of Disease Study suggested that 3.09 billion people had untreated caries in their adult teeth.
If we turn back to the Selig and Silcox study on Microsyops, we’ll see that their Table 1 contains a list of fossil mammal species that had been previously investigated for caries. On the list, we see two hominids, from the Pliocene-Pleistocene and the Mid-Pleistocene, respectively. Look at how frequently these samples—who existed long before serious dentistry was around—had caries:
To figure out what went wrong in our mouths between early Hominidae and today’s Homo sapiens, we have to look at archaeological evidence. A perusal of the relevant literature shows repeated reference to the seminal text on the matter: Cohen and Armelagos’ 1984 volume Paleopathology at the Origins of Agriculture. Cohen and Armelagos mustered data from twenty-one societies to illustrate a trend towards worsening health during the transition to agriculture. In nineteen of those societies, agriculture brought an increase in disease and a reduction in physical stature that we’ve only managed to reverse after the Industrial Revolution.10
There are many reasons for these changes: humans began living closer together and with more animal contact, promoting infectious disease; nutritional quality per person declined as meat was replaced by wheat, leading to numerous observations of osteoporosis and anemia; and through the transition to plant consumption, the dietary environment became conducive to caries. Publications have generally tended to affirm the ill effects of the transition to agriculture.11
One straight forward example of what paleopathologists have learned from skeletons concerns historical changes in height. Skeletons from Greece and Turkey show that the average height of hunger-gatherers toward the end of the ice ages was a generous 5' 9'' for men, 5' 5'' for women. With the adoption of agriculture, height crashed, and by 3000 B. C. had reached a low of only 5' 3'' for men, 5' for women. By classical times heights were very slowly on the rise again, but modern Greeks and Turks have still not regained the average height of their distant ancestors. — Jared Diamond (1999)
Genetic evidence clearly points to the Agricultural Revolution as a critical point for the evolution of S. mutans. A revealing publication from 2012 used sequencing data from 57 S. mutans isolates and three Streptococcus relatives and uncovered evidence that the S. mutans population exponentially increased right around the dawn of agriculture, with evidence for positive selection for fourteen genes implicated in sugar metabolism and tolerance to the higher levels of acid it would produce with humanity’s new diets. The authors noted:
Our estimates for the timing of the demographic expansion in S. mutans coincide with the origin of human agriculture [10,000 years ago]…. Numerous studies in physical anthropology have shown an increased prevalence of dental caries in human remains from post-agricultural societies (5–50%) when compared with remains of Mesolithic hunter–gatherers (0–2%). This pattern has been attributed to changes in diet and the consequent increase in consumption of carbohydrates in human populations after the development of starchy crops, leading to the establishment of infectious agents causing dental caries. Our timing and expansion estimates are consistent with S. mutans as a possible etiological agent of human dental caries; however, it is not possible to rule out other oral bacteria species as also contributing to the development of this disease.
There’s considerable evidence that our dietary niche bred our dental predators,12 and there’s also evidence that the dietary shifts that accompanied the Industrial Revolution have promoted extremely cariogenic bacteria. This makes total sense, because even compared to humans at the dawn of the Agricultural Revolution, we have extraordinarily sugary diets.
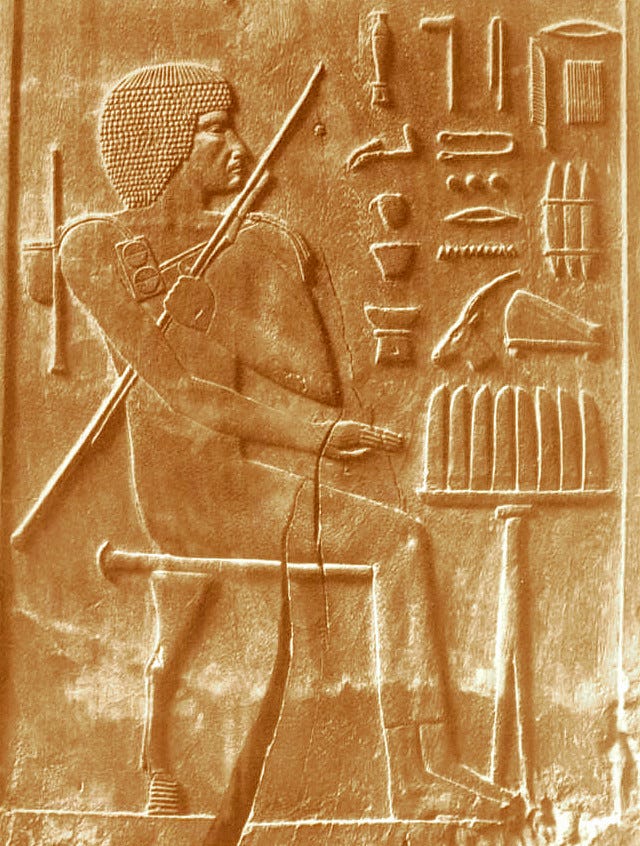
As a species, we’ve socially developed adaptations to caries and other dental maladies, and they’ve been in use for a long time. For example, there are 9,000-year-old dental drillings from the Indus Valley; 6,500-year-old dental fillings made of beeswax have been found in the area of modern Slovenia; from the ancient Egyptians, we have the earliest records of a named dentist, one Hesy-Ra:
The Code of Hammurabi lists dental extraction as a punishment; there are paintings, drawings, and inscriptions regarding dental work going back thousands of years; prosthetics, amalgams, dentures, and orthodontic devices abound in the historical record going back into the B.C.’s. Clearly dentistry has been prevalent in human history for as long as we have records, and it’s no surprise given the importance of the mouth in everyday life and and costs of conditions like caries.
The Human Toll of Mouth Holes
If you live in the developed world, you probably take dentists for granted. If you’re suffering from caries, it’s straightforward to have that problem fixed. All you have to do is pick up the phone, schedule an appointment, and head in to have your teeth drilled and filled, and voilà, you’re fixed.
But like many conditions that we’ve learned how to easily fix, dental caries still exact tremendous costs, and those costs are borne unequally. The CDC has produced handy infographics showing this reality for children, adults, and the elderly. Children first:
Then adults:
And finally, the elderly:
Across all age groups, there are plenty of caries. But while most Americans have the ability to get their caries fixed at a dentist right away, the same isn’t true for many of the billions of other people currently living with untreated caries. A lot of this has to do with the fact that they are poor, mostly by virtue of living in developing countries.
All countries begin poor; so far, only some have become rich. During the process of development, obtaining cheap, sugary Western foodstuffs happens before there are widely available medical services to combat the cariogenic side effects of the transition to the modern, sugary food environment. As a result, when the Third World starts eating like Westerners, the result is untreated dental decay. The stories about this sound fairly horrifying. For example, Cirino and Scantlebury recounted that decay in developing countries “is usually left untreated until it becomes so extensive and/or painful that extraction is the only option.”13 Yee and Sheiham wrote
Three-quarters of the low-income nations do not have sufficient resources to finance an essential package of health care services for the children of their countries…. Although the level of dental caries in low-income nations is categorised as low, requiring mostly single surface restorations, approximately 90 per cent of the caries remains [sic] untreated in both the primary and permanent dentition. Analysis utilising some epidemiological disciplines has demonstrated that to treat dental caries by traditional amalgam restorative dentistry in the permanent dentition of the child population [(most of which reside in the developing world)] would… [require] financial resources beyond the capabilities of low-income nations.
Left untreated, those childhood caries will also go on to become a bigger problem as kids age. The rates of caries may have also increased as development has led to sugary dietary changes outpacing dentistry even further. In some cases, this sort of development has been so severe that entire villages of children have untreated caries.14
The health impacts of caries can be severe. Caries can lead to several types of infections, like abscesses in the root (periapical) or on the gums (periodontal), and these can cause infections that can spread elsewhere in the body, including cellulitis and osteomyelitis. Caries in upper teeth can easily cause sinusitis and all the problems related to that too. In some rare cases, caries can lead to Ludwig’s Angina, endocarditis, septicemia, or cavernous sinus thrombosis. Your teeth are important, and failing to take care of them will result in reduced quality of life and might be your death.
Modern studies have related poor oral health to suicidality, caries have been related to mortality, repeatedly, across races, in fairly select cohorts, and through other proxies like tooth loss. This relationship isn’t likely to be entirely causal, as we might reasonably expect people with low conscientiousness and otherwise poor habits to have more dental decay and to be at a greater risk of dying, but it is consistent with what dental caries do. They certainly do not reduce people’s risk of dying, and the historical record suggests they were associated with high mortality not too long ago. Some related conditions still are, and there are even instances where children in the developed world have died from complications related to caries in living memory.
Globally, billions have caries, and millions—maybe billions—actively suffer from them, while nontrivial proportions of those people end up with tooth loss, infections, chronic pain, generally worsened health, and so on. Historically, caries have been a plague on humanity since the dawn of starchy and sugary diets, and they’ve undoubtedly resulted in millions of casualties. But today, they’re generally not deadly because we have modern dental care, so we’ve forgotten the real, human toll of caries, and we focus too little on the costs they place on poor, infirm, and incapable populations today. To put this in perspective, consider George Washington.
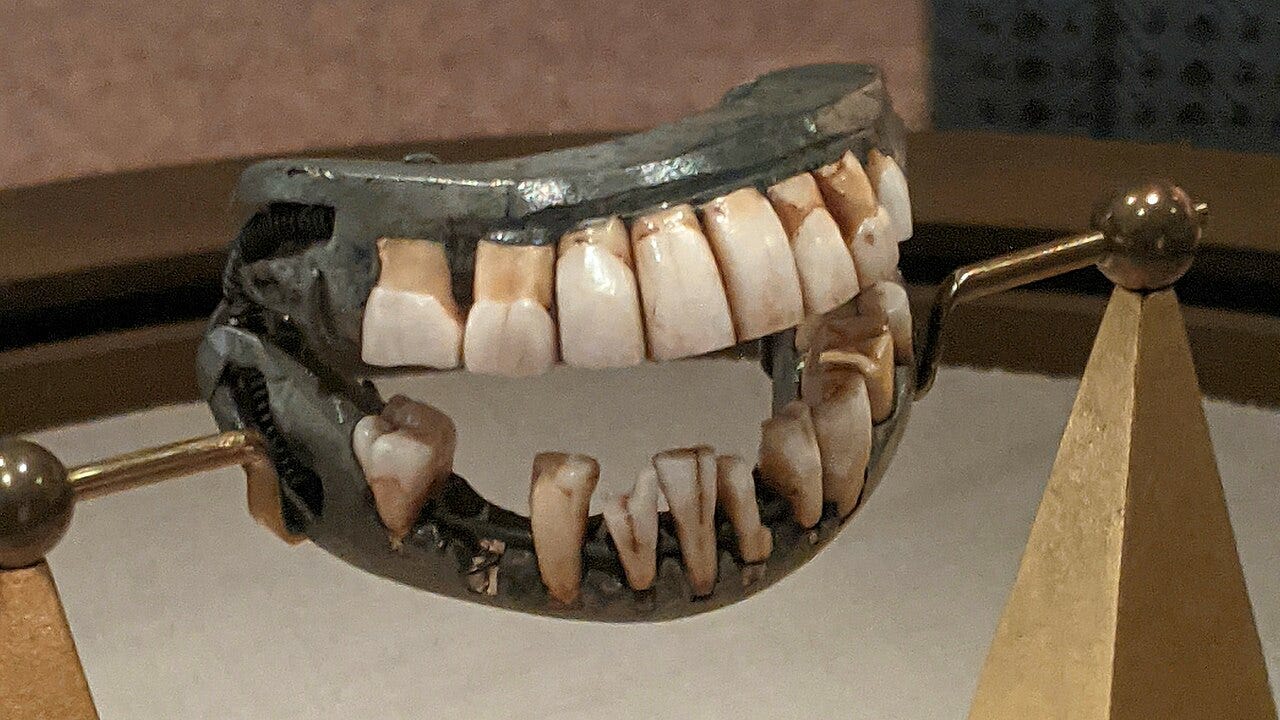
Washington’s teeth started needing to be removed when he was 24 years old. Eventually, he had no teeth at all, so he commissioned no fewer than four pairs of dentures during his lifetime. Washington frequently complained about his dental pain and the pain from his dentures. From their appearance, the pain they’d cause is obvious:
For the Americans, pull out a one dollar bill and look at Washington’s lips.
They do not look normal, and they were not normal.
Washington’s lips bulged out of his face and made him look unnatural, which he often complained about. In fact, Washington spoke with a hiss due to his dentures, and the embarrassment over that might have contributed to his reclusiveness.
Washington was, unfortunately, not unique in suffering from decay and, in fact, among his contemporaries, he might have taken better care of his mouth than others tended to. Many of Washington’s peers preferred to simply live (and sometimes die) with rot. But Washington knew that a leader had to at least have teeth in his mouth, so he lived with the pain.
John Adams had very few teeth due to his love of sweets and his belief that vomiting was good for your health. Consequently, it became difficult to understand him in mid-life because he refused to wear dentures. Thomas Jefferson was renowned for his excellent oral health, as he had only lost a single tooth to decay by the time he died. Paul Revere was well-known as a silversmith, and he was also a dentist!
The stories of the Founding Fathers’ dental conditions could make for much more writing, but I’d rather bring things back to the common man. Or rather, woman. Because the anecdotes you may have heard from your grandparents or great-grandparents about wives having all of their teeth removed and dentures put in? Many people have them and the practice is attested to in the historical record. That’s how bad dental conditions used to be.
More morbidly, have you heard of Waterloo Teeth? After the Battle of Waterloo, scavengers went to work extracting teeth from the dead, as was the fashion at the time for use in bridges and dentures. They were so necessary that this act of desecration was simply accepted. There are many indications that this practice was common for a long time. I assume some of you have visited the Paris Catacombs. The missing teeth of almost all of the skulls down there attest to the commonality of the practice of taking teeth from the dead for use in dental devices.
On the more statistical side of things, the Health Examination Survey in 1960-62 looked at the prevalence of tooth loss among U.S. adults aged 18-79 and it produced a shocking estimate about the extent of dental decay in the American population.15 By the time they tended to die, half of Americans had lost all of their teeth, becoming edentulous. Beyond typical life expectancies, more than half of Americans simply had no natural teeth.
By 2010, this number had dropped to a still high 13%. The health burden of dental decay until very recently has been immense; those reading this are among the first generations that can reasonably expect to enter old age with a full set of pearly whites.
Disease Elimination
Only one human disease has officially been eliminated: smallpox. The last person to have smallpox was a Somali man by the name of Ali Maow Maalin. He survived infection in 1977 while in his early 20s and no one has been observed with the condition in a natural setting since. Given the scale of deaths from smallpox in human history, this is one of the greatest achievements of modern medicine.

We’ve come close to eliminating other diseases, but no other disease has officially been eliminated. Examples include polio, Guinea worm, Yaws, and—in a very geographically-isolated manner—even malaria. Humans have managed to fully eliminate a single other disease, and it’s the bovine disease rinderpest.
Both smallpox and rinderpest plagued humans and their livestock for millennia and they could only be eliminated after vaccines were invented and distributed en masse. The cost of smallpox elimination was undoubtedly worth it to eliminate one of the biggest killers in the history of mankind, and doubly so because it was surprisingly cheap. But the effort was also lucky, since the virus “produced acute illness, had no carrier stage or non-human reservoirs, and had an effective vaccine that was used in combination with international surveillance and public education.”16
Ending other diseases has proved much more difficult despite ample demand.
Are Caries the Latest Disease on the Chopping Block?
When a tool came along to decisively eliminate smallpox, it was gone within a few short decades. The immense human cost of caries has to make you wonder: why haven’t we eliminated them yet? Given the conditions that were needed to drive out smallpox and rinderpest, we have to ask: do we have tools for caries?
Brush your teeth. That’s what you’re supposed to do, but does it work?
Meta-analytically, the people who toothbrush more have fewer caries.17 But that’s what you’d expect if they were also just generally more careful people who follow the generally-accepted ‘good advice.’ Similarly, regular dental care is strongly related to reduced incidence of caries and is uninformative for the same reasons.
Because almost everyone brushes their teeth, it can be hard to know if doing the bare minimum works. So what about some experimental modifications to common practice to suggest what works better? As it turns out, we have Cochrane Reviews aplenty.
High-fluoride toothpaste prevents caries, with some qualifiers about potential fluorosis risk for the young.
The evidence on whether flossing helps is extremely poor. Similarly, there’s weak evidence favoring the use of other interdental cleaning tools and methods like interdental brushes, tooth cleaning sticks, and oral irrigation over doing nothing, and potentially over flossing.
Chlorhexidine mouthwash might be good for gingival health and is certainly good for plaque buildup.18
Overall, the experimental evidence doesn’t show much difference between brushing teeth like normal and practices like using more heavily fluoridated toothpaste, and flossing or using other interdental tools, and it supports using powered brushes, but not to enormous effect, while also supporting the use of mouthwash.19
Or to get back to the point, it doesn’t seem like we have a way to eliminate caries through home practices, but combining the experimental evidence with the observation that fewer people are ending up toothless by their twilight years, it certainly seems like we’ve gone a long way towards that end.
But room for progress remains.
The day is surely coming, and perhaps within the lifetime of you young men before me, when we will be engaged in practicing preventive, rather than reparative, dentistry. - G.V. Black, 1886
What if there was a one-shot solution to dental caries?
Well there is, and it was discovered around forty years ago.
In 1984, through brute force, Hillman, Johnson and Yaphe isolated a strain of S. mutans that produced a novel bacteriocin—bacterially-produced toxins that inhibit growth in other bacteria nearby. Some variants were deficient in producing this bacteriocin and others produced twofold amounts. The ones that produced more of the bacteriocin proved highly capable of colonizing rat mouths.
Late in the next year, one of the discovered strains—dubbed JH1001—was applied to the mouths of five human subjects. The subjects were exposed to three different infection regimes. Three were infected once per day for four days, a fourth was given a dental prophylaxis (to suppress pre-existing S. mutans) and infected once per day for four days and then once every ten weeks for the next 2.5 years, and the final subject was given a dental prophylaxis and two exposures per day for four days. For one subject, JH1001 simply failed to take hold, whereas for another, it disappeared midway through the first year. For the rest, it was variously persistent, and in one subject, it constituted the only S. mutans still living in their mouth by 2.5 years.
In June of 1987, the Hillman group had two more papers published on their S. mutans specimens.
One paper showcased the discovery of a variant of S. mutans that produced acetoin and was lactate dehydrogenase deficient (LDH-d), preventing the bacteria from producing any lactic acid. This is when things start to get interesting. Just three years later, a follow-up on LDH-d S. mutans showed that such a strain failed to produce caries on enamel in vitro, whereas a normal, non-deficient strain rotted enamel exactly like you’d expect. The differences at 10 (normal S. mutans) and 21 (LDH-d S. mutans) days are stark:
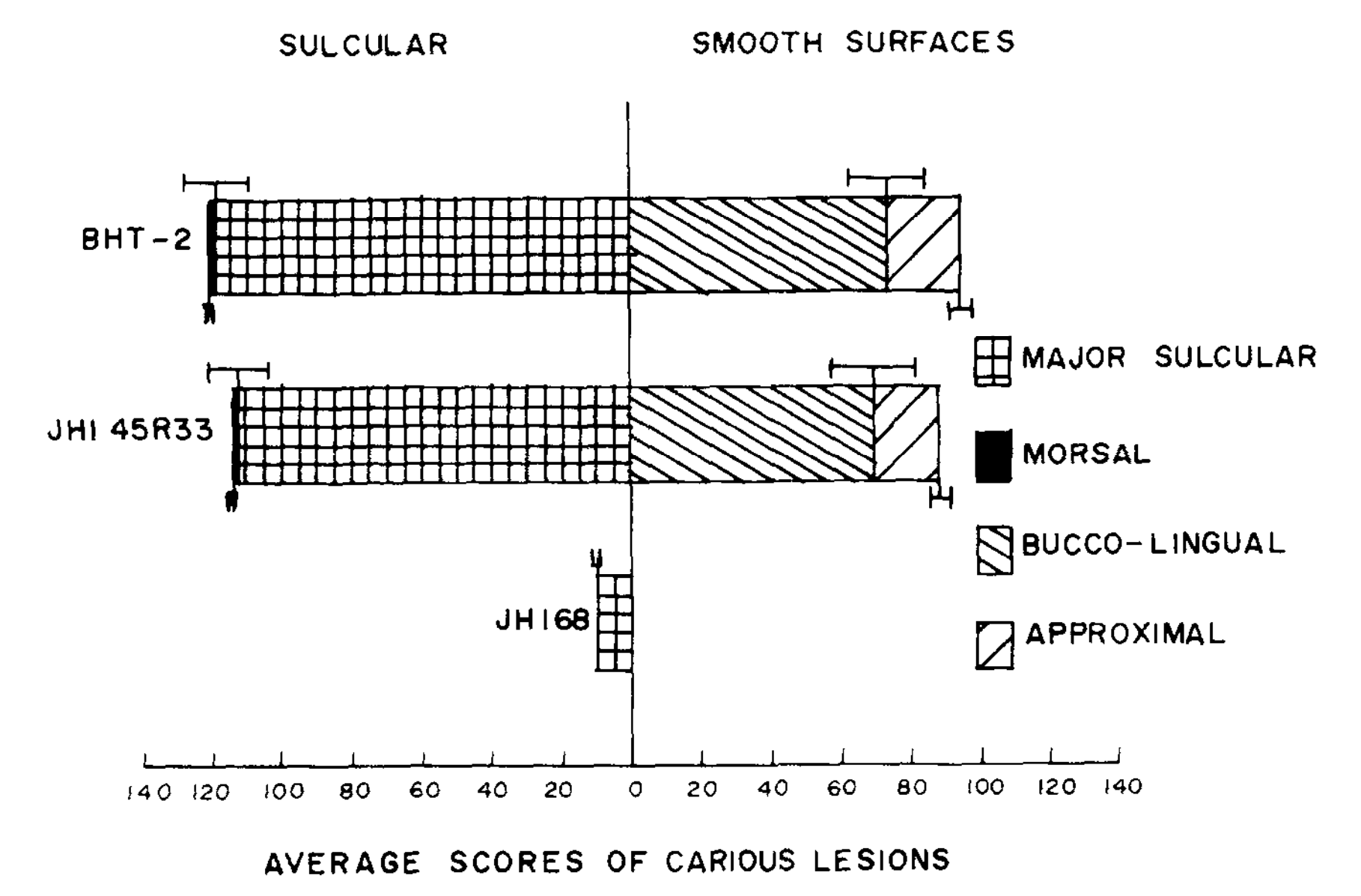
In the paper’s second demonstration, germ-free rats were infected with normal S. mutans (BHT-2) and the LDH-d strain (JH168), in addition to a wild S. mutans (JHI 45R33). The result was staggering: there were basically no caries in the LDH-d strain, but the normal and wild-type strains had plenty of caries after just fourteen weeks:
In the second of the papers from 1987, JH1005—a version of JH1001 with three-times the bacteriocin activity—was shown to successfully colonize three human subjects’ mouths after a single application using a simple procedure. The procedure can be done in the home: polish the teeth with dental pumice, brush the specimen onto the teeth for a few minutes, and you’re good to go. More bacteriocin seems to be all it takes to make colonization work in people who are already living with their own oral microbiomes, rather than like germ-free rats.
All of the key ingredients existed to create a caries vaccine if an LDH-d S. mutans with high bacteriocin activity could be isolated. Fast forward to 2000 and such a strain was being characterized—or rather, constructed.
The Hillman group described the process of taking a super-colonizing strain—JH1140—that produced considerable amounts of the desired bacteriocin (now named mutacin 1140) and making it into a vaccine for caries by making it LDH-d too. Because making S. mutans LDH-d was generally lethal for the bacteria, Hillman et al. opted to trade lactic acid for ethanol by substituting the adhB gene from the bioethanol-producing bacteria Zymomonas mobilis for the S. mutans gene behind its lactic acid production, shifting it from lactate dehydrogenase to alcohol dehydrogenase.
The process of doing this involves swapping the open reading frames for ldh and adh by first deleting ldh through circle PCR mutagenesis and then amplifying the reading frame for adh, purifying, ligating, and transforming to eventually obtain a reading frame for ldh that contains adh. This is then strapped onto a suicide vector called p95 to get the delivery plasmid pTB1002. This is then introduced into a JH1140 specimen to replace its ldh through a heterodiploid intermediate (HD83) that’s grown for twenty generations to enable a recombination event that purges p95 and the original ldh or the new mutant ldh.
Specimens resulting from this procedure were screened and some, without a lactate end-product, were identified.
Thus, the super-colonizing, LDH-d S. mutans BCS3-L1 was born, and the testing proceeded immediately.20
In germ-free rats, the non-LDH-d strain produced caries and BCS3-L1 largely did not:
In Sprague Dawley rats, BCS3-L1 was much better than JH1140, and it was nonsignificantly better than the pre-monitoring verified absent S. mutans controls:
And in terms of its ability to colonize the mouth, BCS3-L1 might have even been better than JH1140. For safety, there were no signs of toxicity, rats didn’t end up with different weights across experimental conditions.21 All signs pointed to this working, and two years later, Hillman described colonization working in humans, with no apparent ill effects, and yet more indications of protection from caries in rats.
Based on the stories I’ve been told, the bacteria has been a total success in the mouths of the Hillman group and everyone else who’s had their mouth colonized by BCS3-L1.
Brighter Smiles Through Biotechnology
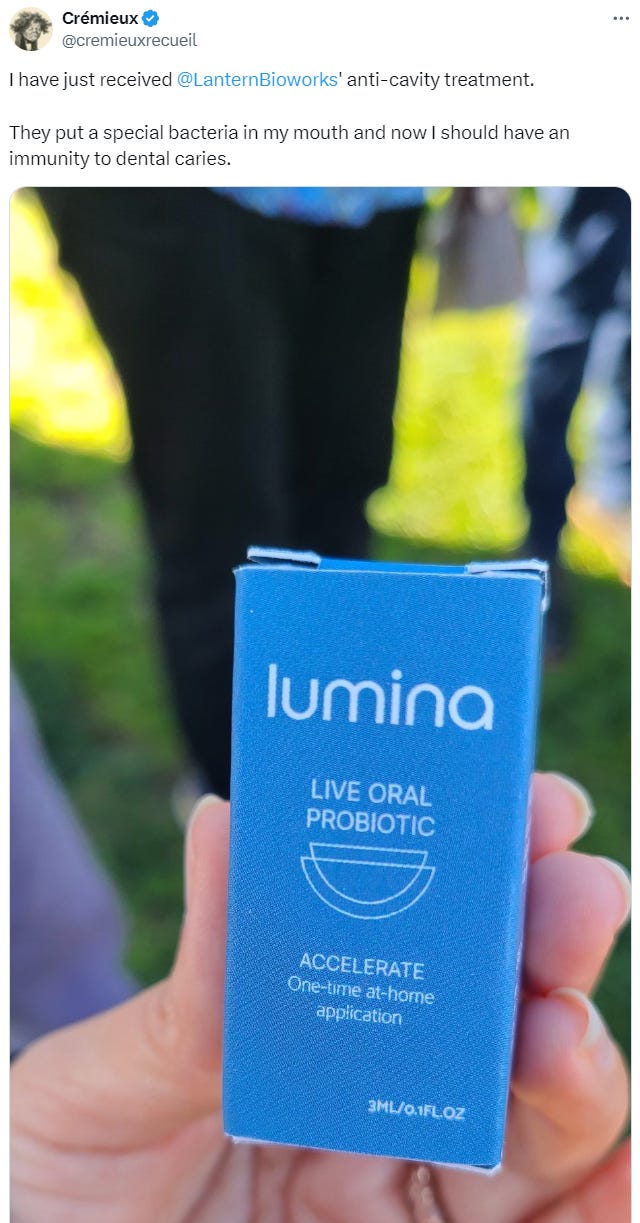
If you’ve been on Twitter lately, you might have seen when I made this post:
I’m one of the latest people to have had this wonderful living caries vaccine applied to their teeth. Given the incredible human toll of caries, you might be wondering when you, too, can get this healthier form of S. mutans in your mouth.
The answer is now. Orders just went live and you can place them here for just $250.
BCS3-L1 will soon be home-delivered in the U.S. for the price of a single dental filling, and there are plans to expand to other locations in the works too. The scourge of poor dental health that has wracked humanity for 10,000 years might soon be behind us.
A lucky part of all of this is that we’ll only need to try our hand at eradication once.
Like smallpox, S. mutans doesn’t have some natural reservoir that will crop up to re-infect humans with a wild strain that brings caries back. After we’ve gotten rid of it, it’s likely that caries will simply be diminished to the point of irrelevance for the vast majority of mankind. What’s more, because of the parent-to-child transmission described at this article’s outset, if a would-be parent is colonized, their kids will end up living a life that’s likely to include far fewer or zero caries.
The benefits for the poor, the old, infirm, and incapable of taking care of themselves, and the Third World are so large that there ought to be a public health initiative to spread this around. Such an effort would ultimately save many billions of dollars and hundreds of thousands, millions, or—in the long-enough run—potentially billions of human lives.
If you would like to read more about BCS3-L1 (also known as Lumina or SMaRT), please see Defying Cavity on AstralCodexTen.
And if you want to buy the product, I’ll link it again with this notice: orders are live and you can place them here.22 We now have the tool to make a long-time human plague disappear. Let’s use it.
Or your father. Ultimately, this is down to proximity and interaction. Since mothers tend to have greater involvement in the early upbringings of their kids, children’s oral microbiomes tend to have greater resemblance to their mothers’ than to their fathers’.
The acquisition of maternal oral microbiota has been observed directly and the pattern of mother-biased transmission has been observed in places as diverse as Finland and Japan, and maternal and, more generally, parental transmission is even acknowledged by mainstream view-reflecting corporate and academic entities. The non-acquisition of the maternal oral microbiome—or, indeed, any S. mutans—has also been noted in scenarios where children are taken care of by caretakers besides their mothers. On a related note, there’s also evidence that couples colonize one another’s oral microbiomes, and it stands to reason that the oral microbiome can be colonized in many other ways, through social, dietary, and other environmental means.
The most extensive paper on microbiome transmission covered both the gut and oral microbiomes and was published very recently. It used data from multiple countries, yielding a reasonably large sample that was more than sufficient to showcase the maternal-paternal oral microbiome colonization discrepancy. That discrepancy is plainly visible in this graph:
This is the main cavity-causing bacteria in humans, but it is not the only cariogenic bacteria.
Because this scenario only involves lactic acid and S. mutans, no other bacterial strains, no saliva buffer, and no remineralization, it is not an exact representation of what happens in the human mouth, but it is illustrative of what happens to humans over longer timespans.
For additional historical details about caries and how their causes were finally discovered, see Ruby et al.
Or on rare occasions, monophyodonts like the rat and toothed whale.
As an aside, there is a well-known myth that Nile crocodiles have their teeth cleaned by birds. This comes from Herodotus and it is neither supported for any crocodiles nor relevant for alligators.
Including various Nodosauridae, hadrosaurs, and—controversially—maybe even oviraptors.
As some have noted, there were likely “frugivores” before the emergence of true fruits following the Cretaceous Terrestrial Revolution wherein gymnosperms were outcompeted by angiosperms. These early fruits in evidence look to be dominantly nuts, and the earliest examples of eating them include gizzards, making them unrelated to the issue of dental caries.
After publication, I was asked if this is more important than the other explanations for why dinosaurs didn’t have caries because ‘HF is obviously bad.’ This is probably not actually a huge concern and I only included it because the buildup of HF was suggested by Lübke et al. (2015), who wrote:
As mentioned above, the reason for the use of fluoroapatite by sharks in their teeth cannot be explained by an increased hardness. A better preservation against bacterial attack (caries) can also be excluded as sharks and marine reptiles regularly change their teeth. For land-living organisms such as the dinosaurs S. maroccanus and C. saharicus, it is particularly surprising that they have used fluoroapatite. This mineral dissolves in contact with acids (such as acidic fruits) below a pH of about 5. Contrary to hydroxyapatite as in human and mammalian teeth, it releases hydrofluoric acid (HF) which is a highly toxic compound. This will be rapidly diluted and removed for sea-living organisms such as sharks, but will remain in the mouth for land-living dinosaurs.
I thought this was funny, so I kept it in even though it doesn’t feel like it’s important and I personally don’t think meaningful levels of HF should accumulate from interactions with lactic acid. But I realize my opinion is not shared by all (including some dentists, one dental researcher, and one chemist I spoke to) and I could be wrong.
Given how fluoride works to strengthen teeth, I thought that paragraph sounded odd. Fluoride both limits demineralization and enhances remineralization. What I thought I knew regarding remineralization was that it creates a “veneer” with “a composition somewhere between hydroxyapatite and fluorapatite…. This new surface will be ‘fluorapatite-like’ in its properties so that the crystal will now behave like low solubility fluorapatite rather than the high solubility carbonated apatite of the original crystal surface.” This new surface is harder than the old one, so “subsequent acid challenges must be very strong and prolonged to dissolve the remineralized enamel.”
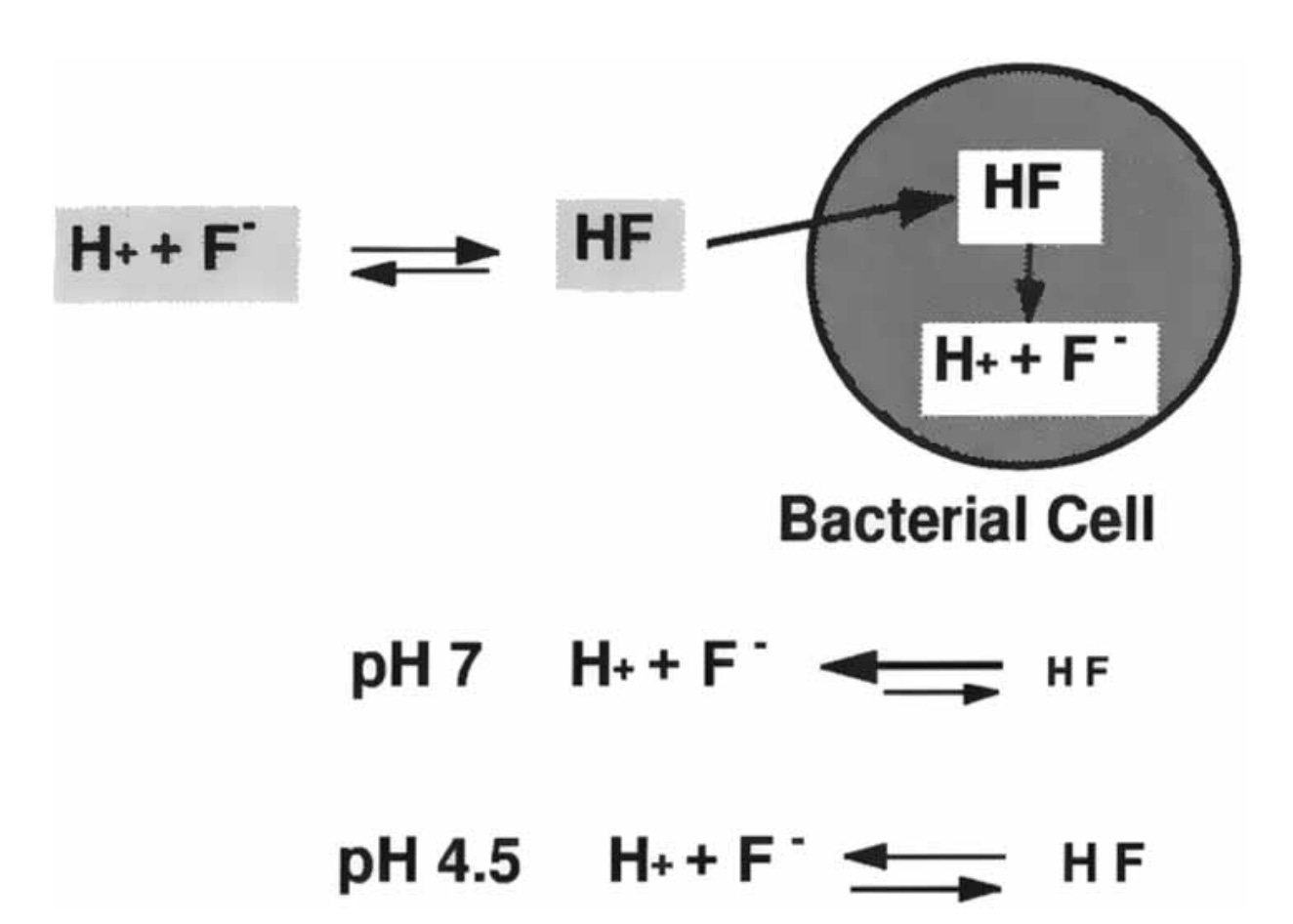
But the reason I might be wrong and HF actually might be a significant concern for dinosaurs could be for the same reason that it’s a concern for the bacteria involved in producing caries. As the paper notes:
Perhaps the most significant findings in several laboratories are that fluoride cannot cross the cell wall and membrane in its ionized form (F-) but can rapidly travel through the cell wall and into the cariogenic bacteria in the form of HF. HF forms from F+ and F- ions as the bacteria produce acids during the metabolism of fermentable carbohydrates. So, as the bacteria produce acid the pH falls. A portion of the fluoride present in the plaque fluid then combines with hydrogen ions and rapidly diffuses into the cell, effectively drawing more HF from the outside and so on. Once inside the cell the HF dissociates again, acidifying the cell and releasing fluoride ions which interfere with enzyme (enolase) activity in the bacterium. Under these circumstances fluoride is trapped in the cell and the process becomes cumulative.
In summary, fluoride from topical sources is taken up by the bacteria when they produce acid, thereby inhibiting essential enzyme activity. This is the third “topical” mechanism of action of fluoride against the progression of dental caries.
HF is at least produced in some quantity, even if it’s not produced in large amounts. The Featherstone paper included a diagram of this process.
It at least seems to be recognized by now that this is an important way in which fluoride protects against caries. A 2017 review on fluoride resistance in S. mutans had the following to say about the antimicrobial actions of fluoride:
The inhibitory effect of fluoride on intracellular metabolism depends on the influx of hydrogen fluoride, which diffuses into the bacterial cells, and dissociates to the proton (H+) and fluoride ions (F-) in the cytoplasm. This process speeds up when the pH of the extracellular environment decreases, as this facilitates the association of H+ and F- to HF. Therefore, even when the extracellular pH lowers, F- and H+ accumulate faster in the cytoplasm, and the antimicrobial effect is stronger. The strong pH-dependence of the fluoride effect is well recognized. The inhibitory levels of fluoride for the glycolysis are as high as 10 mM at neutral pH but are only in the micro-molar range at pH 4.0.
The intracellular F- and H+ can directly or indirectly affect enzymatic activities and physiological processes in the cell, leading to lower acid production, acid tolerance, and adherence of S. mutans to tooth surfaces. It has been found that enolase, which is involved in glycolysis, can be competitively inhibited by F-. This inhibition is observed for purified enolase from permeabilized cells. In addition, enolase is also indirectly inhibited by the acidification of the cytoplasm caused by the accumulation of H+. Moreover, enolase not only plays a role in the glycolytic process, but also catalyses the production of phosphoenolpyruvate for glucose uptake through the PEP-dependent phosphotransferase system. Thus, the inhibition of the enolase activity by F- also has a negative effect on glucose uptake.
S. mutans experiences rapid and dynamic pH fluctuations from pH 7.0 to below pH 3.0 in the oral cavity after dietary carbohydrate intake of the host. The ability of S. mutans to withstand these repetitive cycles of acid shocks is defined as acidurance or acid tolerance. It is one of the major virulence factors of S. mutans. In the presence of fluoride, this ability has largely diminished. The glycolysis of S. mutans stops at pH 6.0 in the presence of 10 mM F-, while in the absence of F-, it is only inhibited at a pH lower than 5.0. The survival rate of S. mutans after exposure to a lethal pH (3.5) decreases 77% in presence of fluoride (5000 mM). The acidification of the cytoplasm via the influx of HF as well as the inhibition of the proton-extruding F-ATPase, accounts for the reduction in acidurance of S. mutans….
Fluoride can affect the adherence of S. mutans to enamel, which is a cariogenic trait of S. mutans. Yet, there is no consensus on how much fluoride influences the ability to adhere. While an obvious decrease in adherence of S. mutans to hydroxyapatite was found with 500 ppm (26.3 mM) F- or even less in some in vitro studies, others reported hardly any change in adherence with >5,000 ppm (263 mM) F-…. Whether the fluoride inhibition of the adherence of S. mutans contributes to caries prevention requires further studies.
In addition to the abovementioned actions, other mechanisms may play a role in the antimicrobial activity of fluoride. Recently, fluoride was found to inhibit alkali production. This is due to the inhibition of either urease or the arginine deiminase system. The former is very sensitive to fluoride, with 50% inhibition by 0.3 mM F-. The ADS, however, is less sensitive than the urease system, and its inhibition by fluoride requires low pH values. Fluoride can also affect metabolism by binding to pyrophosphatase in the presence of Mn2+. Pyrophosphatase is responsible for the release of pyrophosphate from nucleotide triphosphates and is therefore involved in a variety of physiological processes, including biosynthesis and regulation of metabolism.
The importance of HF was mentioned a few times in the above, but I quoted more of what they wrote to emphasize that fluoride may have other means of acting as an antimicrobial. There is more literature on this and other means through which fluoride acts as an antimicrobial, but I believe this is sufficient to make a point.
Because I am open to the possibility that HF matters more than I think it does, I will maintain this part of the article unless someone can present some reason why it’s wrong. In that case, I’ll strike it out, this note will remain, and the new evidence will be linked here.
We see similar diet-caries correlations in other primates, like Gigantopithecus blacki, or even in omnivorous bears like Arctodus simus.
Also interestingly, we see caries in contemporary primates and they’re concentrated among species that eat sugary foods and on the anterior teeth, consistent with practices like “wadging,” where chimps will hold something like a fig, honeycomb, or a bundle of berries in their front teeth to eat, like so:
Areas for progress to be made remain in the less developed parts of the world.
Confirming that the caries findings have to do with the dietary niche, hunter-gatherers with starchy diets have also had lots of caries before the Agricultural Revolution. This is an indication that the association of caries with the Agricultural Revolution is due to the dietary changes it involved rather than the timing alone.
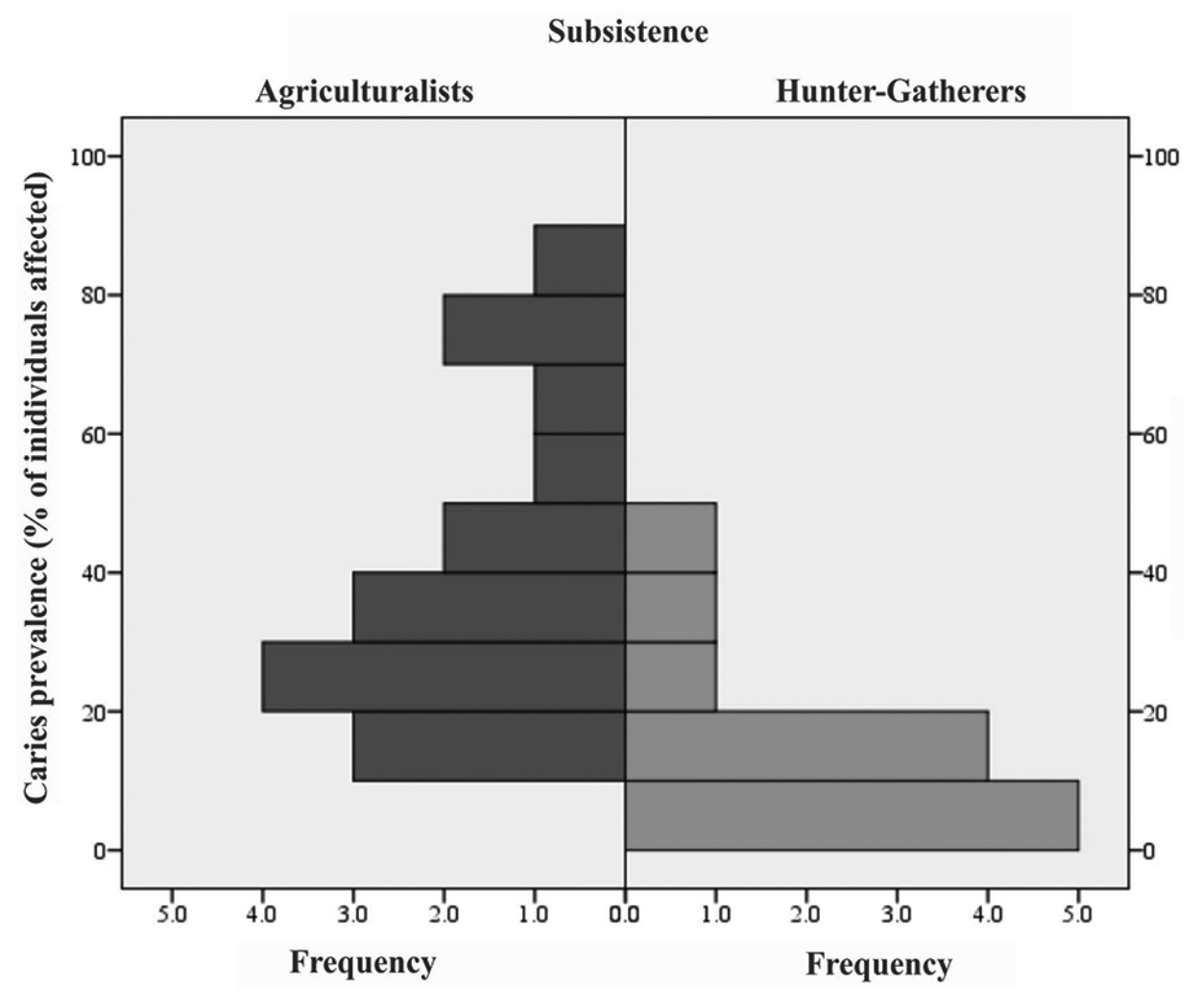
Marklein et al. (2019) provided a good illustration of the differences in the frequency of caries between hunter-gatherers and agriculturalists across 185 archaeological sites:
The graph shows that very agricultural society had caries, but the modal hunter-gatherer society did not.
Nowadays, this is the standard narrative and figures often illustrate the assumptions of this narrative by describing the evolution of S. mutans as a co-occurrence with the dawn of agriculture.
In some places, they’ve attempted traditional remedies for caries, but those traditional approaches “have met with marginal success.”
The most famous case of globalization impacting the food environment doesn’t have to do with caries but, instead, with niacin deficiency—pellagra. In fact, pellagra epidemics resulting from nutritional globalization are the reason we know what niacin is.
In the New World, several populations were dependent on maize (corn) for large proportions or practically all of their diets. Relying on corn for your diet is a recipe for ending up with a niacin deficiency since it contains far too little to survive on in a biochemically available way. But despite that, New World populations didn’t simply exist with high levels of pellagra all the time. They weren’t adapted to go without niacin either. They used a food preparation procedure called nixtamalization to treat corn with slaked lime or plant ash to make the niacin in it bioavailable to humans. This procedure makes it possible to live off of corn without succumbing to pellagra.
In the 16ᵗʰ and 17ᵗʰ centuries, pellagra became a major problem among the north Italian peasantry after corn was imported and people realized it was an incredibly cheap way to produce flour. The reason is that corn was imported without also importing nixtamalization. Since no one knew why nixtamalization was needed, no one thought to encourage it.
In the late-19ᵗʰ century, Christiaan Eijkman was studying beri-beri, a neurodegenerative deficiency of vitamin B1 that was common in southeast Asia. Eijkman found that having the disease was more prevalent among individuals whose diets relied on polished rice, inspiring him to hypothesize that polishing removed an antitoxin that protected against the disease. Shortly after this, studies on voluntary prisoners in Java demonstrated that beri-beri was attributable to a dietary deficiency. The scientist behind these studies proposed that vitamin B1—thiamine—was the cause and that beri-beri could be remedied by supplying this “vital amin” (an alternative spelling of “amine”)—the origin of the term “vitamin.”
Scientists now had an appreciation of the role of nutritional deficiencies in disease.
Later on in 1937, Elvehjem et al. used a corn-fed dog model to demonstrate that supplementing niacin could cure their black tongues and then they applied this to pellagra patients in the U.S. and Italy, curing them of their pellagra. But that wasn’t a sufficient demonstration, as the patients were hospitalized and cut off from other potential causes of the condition. So the Consiglio Nazionale delle Ricerche started seeking out people with pellagra in natural settings and offering them oral and intramuscular niacin as part of a trial. The tongue and mouth lesions, the skin lesions, and the anorexia quickly came to an end. The source of pellagra was discovered after 400 years of suffering, and now the condition is virtually nonexistent in Europe.
For further reading on the history of pellagra in Italy, see Mariani-Costantini and Mariani-Costantini, and for more on globalization and health, see Verginelli et al. A famous book documenting changes in dental quality—among other things—after the introduction of the Western diet is Weston Price’s Nutrition and Physical Degeneration.
I discovered this report thanks to seeing the numbers on this page and thinking they were so unrealistic that it motivated me to track down the source, confirming that they were, in fact, correct.
There was also less public resistance to vaccination for smallpox than there is to certain other common disease vaccination campaigns today, although there was still resistance and vaccine skepticism. Conspiracy theories about vaccines remain, and many misconceptions have been brought forward to maintain the tenability of vaccine skepticism, like through claims that some vaccines are “not vaccines” because they don’t fit a contrived definition of what constitutes a “vaccine.”
It’s worth noting that this study found a larger effect for deciduous than for permanent teeth. It’s not clear why this is, but it could make something out of the London Bills of Mortality. In those, the word “Teeth” is used to denote the death of someone young, a name given because of the recent eruption of their deciduous teeth. People in those ages had excessively high deaths for many reasons, and in some scant records, that reason was explicitly noted to be dental decay.
I suspect powered brushes look more favorable than manual brushes in part because so many of them have time monitoring settings, so people end up using them for longer than they do manual brushes.
Notably, BCS3-L1 has been subjected to some additional knockouts to cripple its horizontal gene transfer machinery, making it likely the most stable S. mutans out there.
The cavity-riddled JH1140 rats were a bit lighter than the BCS3-L1 or control rats, but that wasn’t significant.
It shouldn’t need to be said, but I have no financial conflicts of interest in linking to this product. I am simply happy that a problem plaguing humanity can now be greatly reduced and, perhaps, eliminated.




















I had poor oral hygiene in my 20's. I didn't floss. And it became a problem by my late 20's- I had to have a root canal, another tooth needed a crown. Now, I'm almost 40 years old and I've rarely gone to the dentist over the last 5 because I floss and use a dental pick so thoroughly, I do not require much cleaning when I do go and I obviously have no cavities.
So, I am extemely skeptical of any claim that flossing doesn't work. Of course, you have to flossing properly and I actually remove far more food from my teeth with a pick-- I use those disposable flossing with floss on one end and a pick on thr other.
I created a reddit community to follow Lantern bioworks progress, etc, if you are interested: https://www.reddit.com/r/lanternbioworks/