Your Allergies Are Probably Fake
You might be avoiding medications that don't do anything to you
This was a timed post. The way these work is that if it takes me more than one hour to complete the post, an applet that I made deletes everything I’ve written so far and I abandon the post. You can find my previous timed post here.
For three-quarters of my life, from about ages 6-7, I seriously thought that I was allergic to guaifenesin and dextromethorphan. I’d always been told that I was allergic to these drugs and that they cause me to go into anaphylactic shock.
But that was wrong. I’m not allergic at all. In fact, I don’t have any allergies!1
Millions of people are probably in the same boat I was, albeit with different drugs listed for their allergies.2 The most common example of this—but by no means the only one—is penicillin.
Some six to ten percent of people have been labeled allergic to penicillin, but it’s likely that at least ninety to ninety-five percent of these labels are incorrect and the labeled individuals do not actually have a penicillin allergy. Nevertheless, these false labels result “in unnecessary avoidance of β-lactam antibiotics, leading to worse clinical outcomes, increased rates of Clostridioides difficile infections and multidrug-resistant organisms, greater health care costs, and longer hospital stays” for millions of people each year.
‘How does this happen?’, you might ask. People are usually mislabeled through an abundance of caution. Doctors frequently see something minor, like a skin rash following administration of an antibiotic when they see a patient with an infection, and in order to ensure it doesn’t happen again, they just mark the patient as allergic to that antibiotic. This is usually benign, and most doctors don’t give it a second thought. But, as noted above, this is bad for public health, so we really ought to care.
‘But how can we fix this?’, you might wonder. Well, it’s easy. We need to get systematic about delabeling—the process of testing whether people are actually allergic to something like penicillin, guaifenesin, dextromethorphan, pollen, some random drug or various foodstuffs, and so on, and then removing that label from people’s records if it turns out they don’t react.
The testing is very simple and applies to most drug allergies. I’ll describe my case.
After looking at how uncommon the allergies I thought I had were, I took to looking up the details of my case. In mine, there was nothing that would positively differentiate guaifenesin from dextromethorphan, and both were extremely rare allergies, that have no reason to occur alongside one another. Therefore, it was unlikely that I had both allergies. So, I grabbed a handy-dandy epinephrine pen (just in case) and sat down for a supervised ‘direct oral challenge’: I took a pill containing just guaifenesin, at the highest available over-the-counter dose, recorded the time, and sat, for two hours, monitoring symptoms the whole time.
After two hours, I had no hives, no angioedema, no wheeze, no cough, no hypotension… nothing. By two hours, such a lack of reaction makes it extremely unlikely that I’m truly allergic, and virtually impossible that I have anything like a severe, life-threatening allergy. So next, I repeated this on my lonesome, and again, no reaction. Therefore, I concluded, I do not have an allergy. Whatever resulted in that label being added to my file, it was in error.3
This finding weakly lowered the prior odds that I had the other allergy on biological grounds and it moderately reduced the odds on case-history grounds. So, the next day, I did another supervised direct oral test, this time with dextromethorphan, and two hours later, nothing! Then, I took more on my lonesome and, once again, nothing. I’m not really allergic to either drug!
If people did tests like these, they could get delabeled for most of their medication allergies, and they could benefit from being able to use those medications as a result. The benefits of this wouldn’t just be personal, they’d be social, as less effective care for things like infectious diseases means more spread and longer periods of suffering. If we get people delabeled, we can waste less money on poor-performing medicines, reduce human suffering, and more effectively curb the risk of many common diseases.
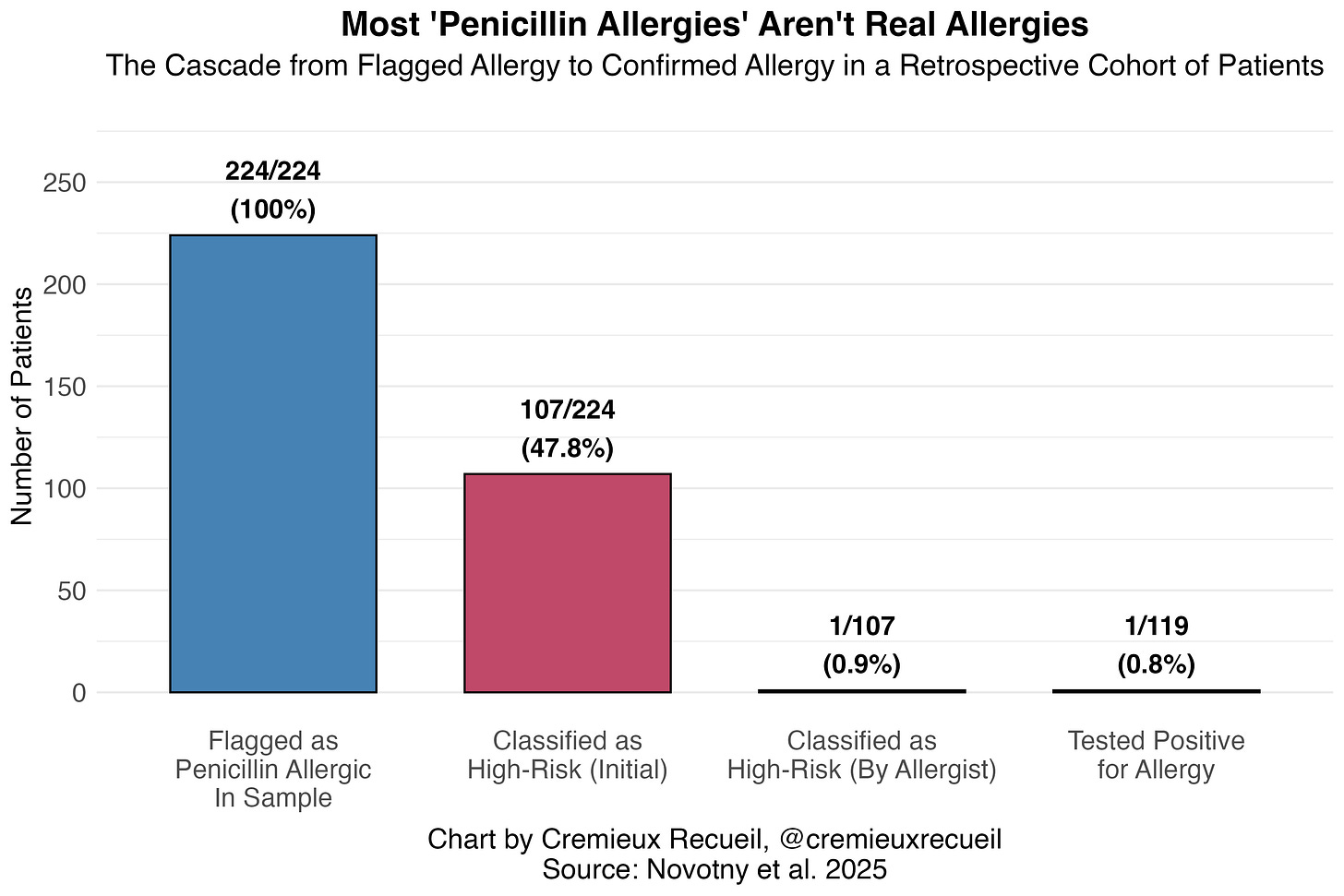
Consider this result for the commonly prescribed antibiotic penicillin: about half of the people flagged as having penicillin allergies in their electronic health records were classified as high-risk, but only one person looked high-risk on allergists’ review, and just one actually tested positive for their allergy!
Penicillin allergies (like so many others): commonly labeled, uncommonly verified. If there’s an annoying allergy with a dubious origin in your medical file, consider going to an allergist and taking a supervised test.
That I’m aware of.
It is extraordinarily rare to be allergic to guaifenesin or dextromethorphan. Only a few cases of each have ever been reported or recorded into individuals’ electronic health records. This rarity is part of what convinced me that I was unlikely to actually be allergic.
Another possibility is that I ‘outgrew’ my allergy, but I doubt this. People often describe this phenomenon, but what they’re likely describing given the biology of allergies is that they never had the allergy in the first place, and they were just mislabeled from the start.


Ever since I was a little kid my parents told me I was allergic to penicillin. They said my tongue went black after a round of it. I planned on visiting South America in 2020 so I had myself tested in 2019 since it is the most common antibiotic and low and behold, I am not allergic to it. I haven't made it to Brazil yet, something happened in 2020. I forget what that was but I am not allergic to penicillin.