Early-Onset Cancer Fast Facts
Are more young people getting cancer? Are more young'uns dying of cancer?
This was a timed post. The way these work is that if it takes me more than two hours to complete the post, an applet that I made deletes everything I’ve written so far and I abandon the post. You can find my previous timed post here.
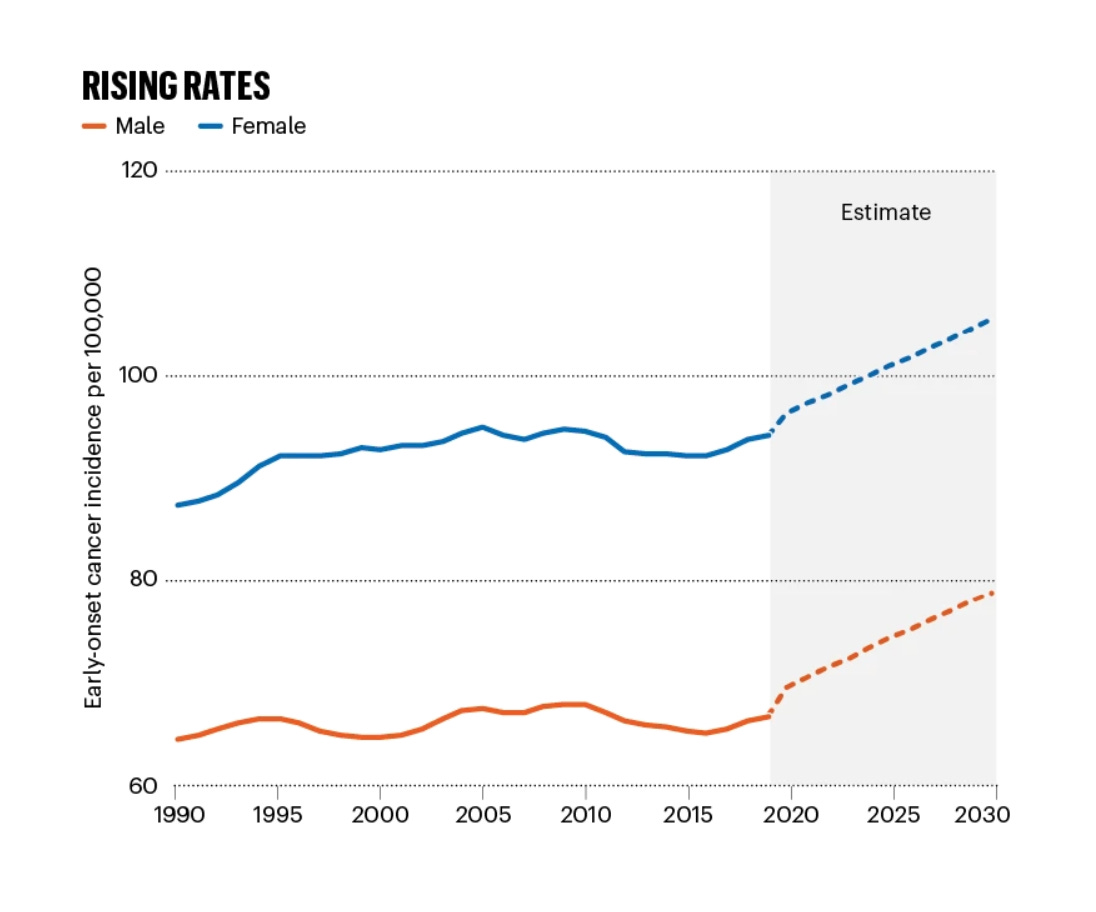
After about 2000, different sources started to agree that the incidence of many common types of cancers had begun increasing. For early-onset cancers (diagnosed in ages 20-49), the increase in high-income countries looked like this between 2000 and 2010:
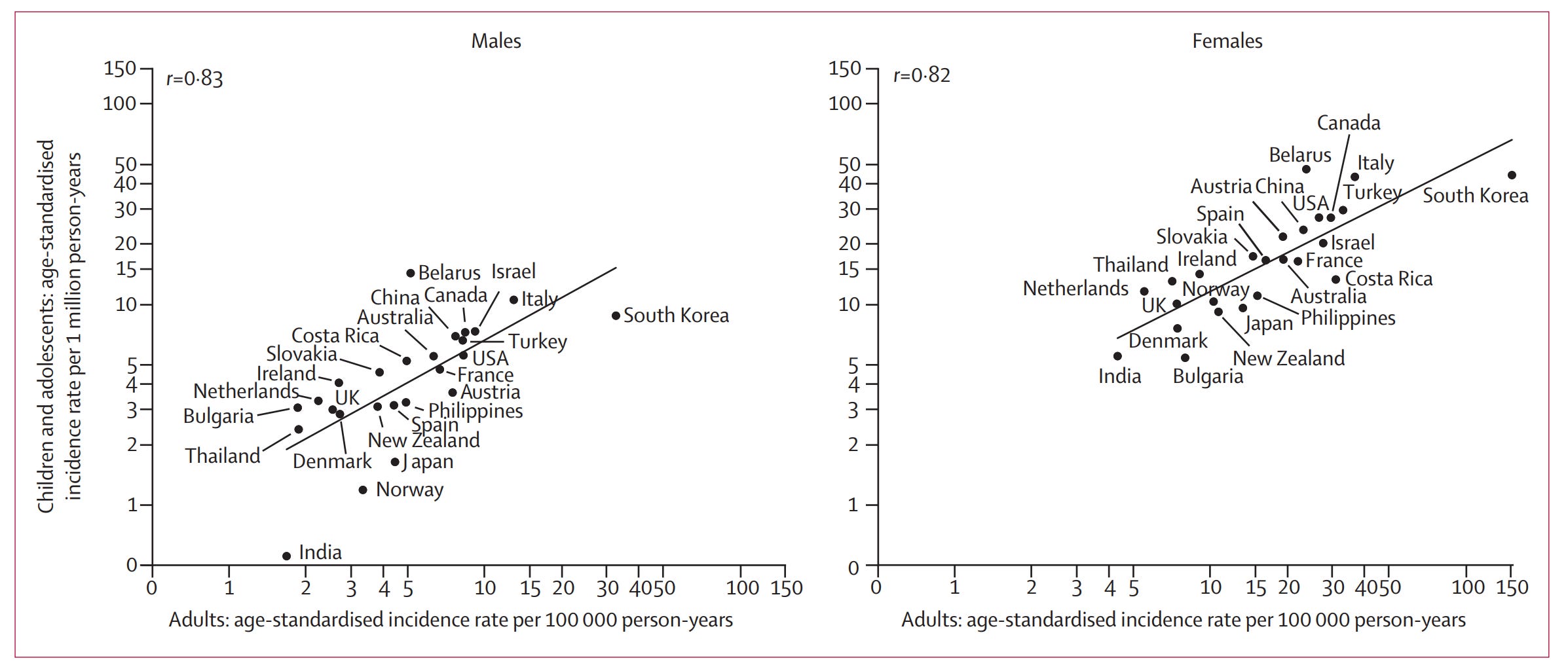
Trends in obesity-related cancers were far more dramatic for both sexes than were trends in non-obesity-related cancers.1 For males, there was no aggregate increase in cancers not related to obesity, and obesity-related cancers increased by an average of 3% per year from the low base rates associated with early-onset cancer. For females, the incidence of both types of cancer increased, but non-obesity-related cancers only went up 1% per annum and obesity-related ones went up 7.4 times more rapidly in percentage terms; in absolute terms, the increase for females was almost four times as dramatic for obesity-related cancers.
Trends are not exactly cut-and-dry, however. This is how early-onset diagnostic trends look in the Global Burden of Disease Study 2019:
With the disruptions to healthcare provisioning brought on by the COVID pandemic, these projections did not hold up: more and more people began avoiding diagnosis, and the naïve view suggested that cancer was declining. But remember, this is just a disruption to diagnoses, not a break in the underlying incidence of cancer. The key thing to remember about all this, however, is that there does not appear to have been a rebound in diagnoses. Typically-cited data remains delayed by several years, but nevertheless, the expected rebounding that should have taken place in 2021 apparently did not occur. I return to the question of rebounding below.
Thus far, I’ve only mentioned diagnoses. Diagnoses are an important bellwether, but they are not enough because there are very many reasons why they might trend. To really understand cancer trends, we have to look at two other factors. Namely:
Disability
Death
Let’s start with disability. Cancer treatment is grueling. If drugs could only be approved on the basis of safety rather than a mixture of safety and efficacy, then cancer drugs would almost never be approved. While most frontline options do work to help people live longer and even cure their disease, they generally do so at great cost to health. Everyone knows about chemotherapy making people bald, brittle, and bony, but such is the cost of survival.
If the incidence of cancer has increased, and treatment has risen with it, then it stands to reason more people might end up debilitated not just by the disease, but by the treatments for it. Using data from the Global Burden of Disease Study 2019, we can answer in the negative: disability—quantified by disability-adjusted life years or DALYs—has not increased among the young. I’ll illustrate this in two ways. The first is to look at total cancer-related DALYs per 100,000 in high-income countries.
A quick glance at this graph shows a worsening situation for every group except the youngest, whose DALYs have declined from 9.99 in 1990 to 6.73 in 2019. This seemingly answers our question, but it leaves behind an overall picture that’s quite dismal. But it is not so, for a simple reason: compositional change. I’ve previously discussed this issue in the context of education and IQ scores, but if you don’t want to go read all that, don’t fret, because I’ll make this simple: the picture here is actually quite nice when we quantify it our second way, by assessing the joint effects of population aging, population growth, and changes in age-specific DALYs.
Aging and growth are benign causes of an increase in DALYs. For the federal government, increasing DALYs are a fiscal challenge, but from the perspective of its its health authorities, they are merely facts to be recognized and for research priorities to be built around, but not things to get especially worried over.
We now have our answer on disability—it’s generally falling across ages, while DALYs rise in total because the population is growing and people are getting older at a rapid rate—so it’s time we moved on to the more morbid and concerning topic of death. The story for early-onset cancer deaths is, once again, seemingly not all that alarming:
The story here is complicated—as in the case of DALYs—by the fact that the population has grown. Deaths from early-onset cancers may be down per 100,000 persons, of which the rates have been somewhat flat, but the number of people getting these has skyrocketed as the global population has done so. The increase in global early-onset cancer deaths between 1990 and 2019 is 28% versus global population increasing 47% in the same period.
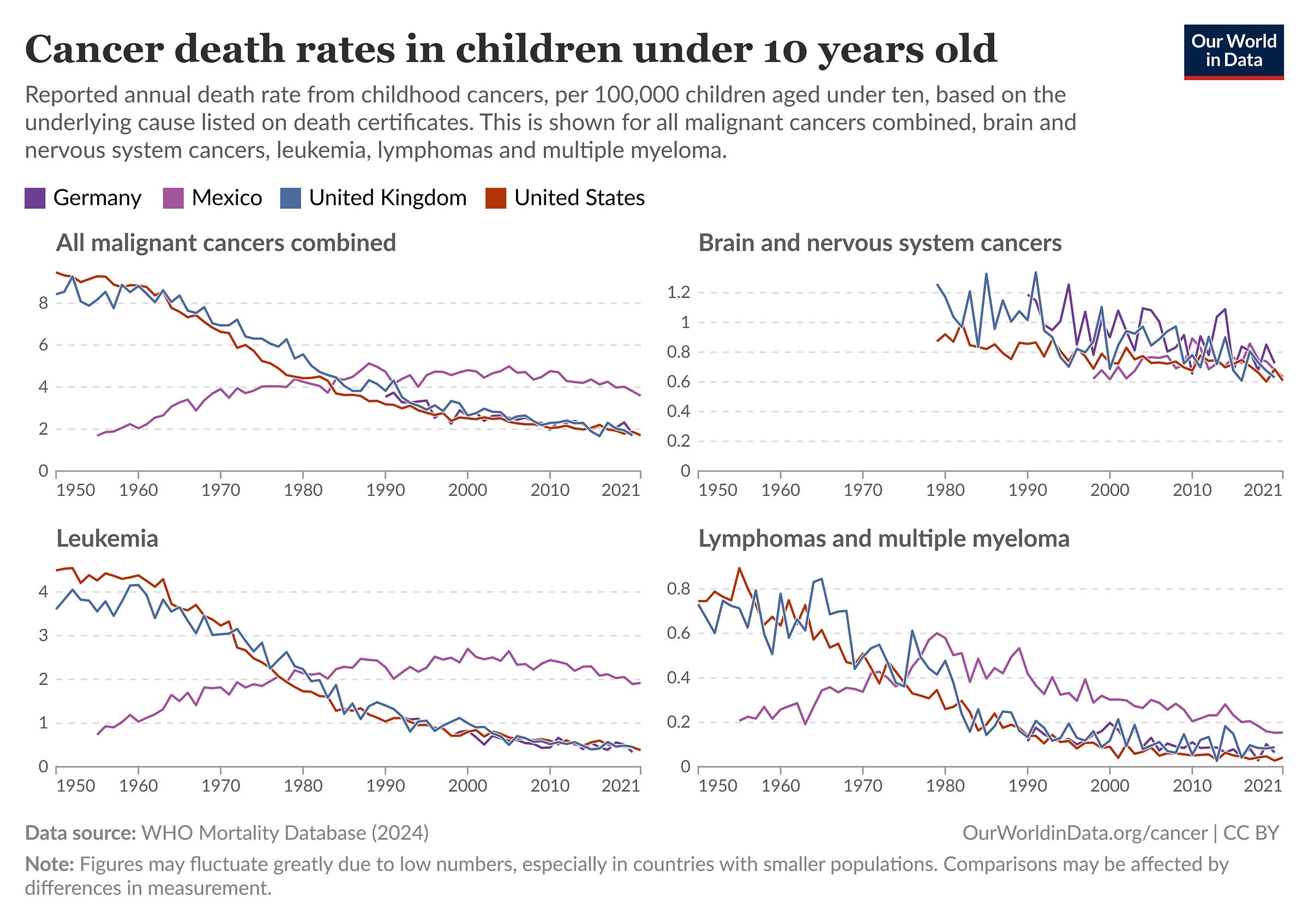
More to the point, in America, Britain, and Germany, cancers for children have declined precipitously. Focusing in on the U.S., the total cancer death rate for those aged 0-4 was down 29.8% between 2001 and 2021. For those aged 5-9, it fell a similar 29.9%, while for kids aged 10-14, it fell 14.7%, but that was 17.6% between 2001 and 2011, so there was some nonsignificant reversion—remember, base rates for childhood cancer are very low. Finally, for youths aged 15-19, the rate fell 23.2% between 2001 and 2021.
A more general picture of cancer death rates provides an estimate that’s further from what we’re looking for, but one which should nevertheless help inform our thinking about cancer deaths.
Across various sources, the picture for incidence is a largely flat or slightly increasing one while the picture for deaths is a mostly joyful one. This is true in the Global Burden of Disease Study 2021 as well, where the age-standardized incidence rate rose 4.1% between 1990 and 2021, while the age-standardized death rate fell 24.1% between 1980 and 2021.
In short, there is no early-onset cancer epidemic. Early-onset cancers are being diagnosed somewhat more often but are still rare in absolute terms, while disabling people less often, and killing far fewer people on a per capita basis than they once did. Hype has distracted from recent, positive trends.
What About Specific Cancers?
The general prognosis for cancer among the young is good and it has improved significantly over time, but one could make the case that while this is true in general, the case for particular cancers is becoming much worse. There is something to this concern, but it has to be tempered. I’ll provide a few examples and some thoughts to chew over.
Thyroids, Melanomas, and Other Cautionary Tales
Melanoma is common, well-known, and generally comes with a good prognosis— especially if it’s noticed early. The adjusted lifetime risk of developing a melanoma increased substantially for American Whites between 1975 and 2018, despite declining time spent outdoors. For men, this increase was a doubling from 3.2% to 6.4%, and for women, it was a near-trebling from 1.6% to 4.5%. Melanoma diagnosed in situ—meaning an early-stage diagnosis confined to its original site and without spread—also increased substantially, from 0.17% to 2.7% for men and 0.08% to 2.0% for women.
Alarm bells should be going off. The distribution of melanoma diagnoses shifted from one marked by relatively few of the less severe, in situ variety of diagnosis, to one where some 79% of the growth for men and 66% of the growth for women was due to just that. Given its apparently declining severity, melanoma has very likely been undergoing a trend towards overdiagnosis. That is, the incidence has increased, without an accompanying spike in mortality as our predilection for diagnosis, our concerns about lumps, our understanding of what’s a freckle and what’s a cancerous growth, and our desire to bill for pro forma excisions at first sight, have all increased. Or in the words of the study’s lead author, we’ve witnessed a move towards overdiagnosis in the sense of “the diagnosis of cancers that meet the pathological definition for cancer but are not destined to cause harm—even if left untreated.”
The evidence for overdiagnosis is not just based on the change in the types of melanoma being diagnosed. It also comes from facts like the mortality rate remaining flat over a period in which incidence rose multiple times over, and the attendant fact that, until 2011, treatment barely changed and until 2014, the effects of improved treatment were barely able to make a dent. Since treatment should make a difference when well-targeted, that it fails to do much in real-world settings suggests it’s being applied to many cases that are insufficiently severe. In an earlier study on the same topic, different methods found similar conclusions: no matter how you slice it, melanoma is increasingly overdiagnosed.2
The pattern observed in the case of melanoma is a common one, and whenever you see it, you can infer that other types of cancer are likewise being overdiagnosed. Just because there’s a lump does not imply it will become debilitating or lethal, but we’ve become more likely to be aware and to treat anyway. That’s simple, so remember it.
If you return to the graphs in the first section, you’ll see that the melanoma-like pattern does not apply in the case of early-onset and other cancers, for which mortality isn’t flat but is instead falling, and for which incidence is either flat or marginally increasing. In those cases, we’re not entirely seeing overdiagnosis. In the general case, we may well be seeing increased diagnosis pushing down death rates. On the other hand, the lack of a post-COVID rebound in diagnoses and deaths suggests that we still need to be concerned about overdiagnosis since pushing down diagnoses did not translate to an abrupt increase in death and disability. But more time needs to pass to fully understand how this observation will hold up, so I digress.
The WHO recently highlighted another case of overdiagnosis, but this on is focused on children and adolescents rather than adults. The researchers behind this work observed that thyroid cancer in those aged 0-19 was rare prior to about 2000, after which incidence began to skyrocket. The evidence that this reflected overdiagnosis was a few-fold.
For one, the features of thyroid cancer observed among youngsters were similar to those observed in adults—and not just in terms of incidence—, for whom we know overdiagnosis is important. How do we know overdiagnosis is important for adults? Because of the melanoma pattern: for adults, diagnoses are being driven by a relatively nonlethal variety of thyroid cancer—small papillary carcinomas—and mortality rates have remained low and stable, or even declined somewhat in most places. The incidence is certainly up, but the mortality rates are flat.
For two, increased levels and quality of surveillance of the thyroid gland are a known phenomenon. New diagnostic procedures like neck ultrasonography have made detection of smaller and smaller, and less and less clinically significant cancers more possible than ever before. The number of indolent, nonlethal tumors known to exist in people of all ages without consequence is being met with higher detection and resultingly more surgeries to remove them.
For three, diagnosis rates appear to be greater in healthcare settings that are more poorly regulated. What this speaks to is that providers may be financially incentivized to diagnose. It makes them money, but this diagnosis can have devastating, lifelong consequences for the patient. The consequences of the surgery or radioactive iodine treatment—which are preferred to untreated, active surveillance for little good reason—are often having to go on lifelong thyroid hormone replacement therapy and suffering through vast reductions in quality of life because the therapy fails to match the quality of having a functioning thyroid.
There are bountiful other examples of increasingly overdiagnosed cancers that may actually be causing harm via their recognition. Many overdiagnosed cancers are tied to discrete changes in diagnostic practice or technology availability. For example, childhood brain tumor incidence between 1973 and 2009 is marked by stability after the mid-1980s, but during the years in which MRIs were introduced (1983-87), there was a rapid, 53% increase in incidence. Changes in classification, registration, and coding have also affected rates for and diagnosed types of childhood brain tumors. Keep in mind that, as shown above, mortality declined across the childhood brain tumor category.3
Similar findings have been made for pancreatic and kidney cancer, hematologic cancers, and more. In short, there is considerable risk of overdiagnosis, even among the young. There is also evidence for improved diagnosis that saves lives but increases apparent incidence, and there is also a staggeringly increasing burden derived from obesity and other chronic diseases wrapped up with obesity. However, despite the growing burden of obesity-related cancers, they have not resulted in the trend towards declining death rates across all early-onset cancers being reversed.
Colorectal Cancer: We Have A Preventative. Why Aren’t We Using It?
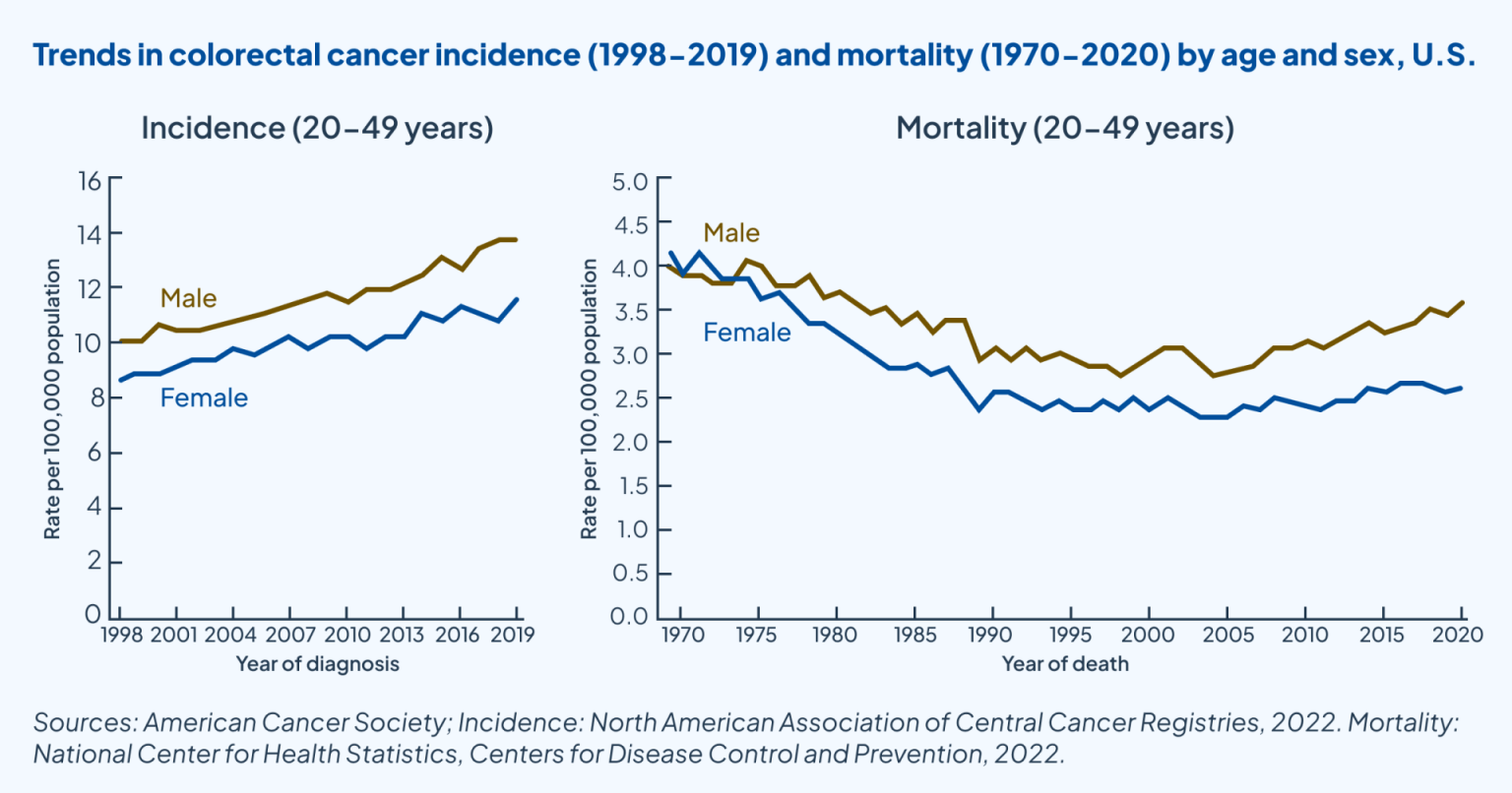
Early-onset colorectal cancer is exceptional. Its incidence has been steadily rising since 1998 in both sexes among those aged 20-49. At the same time, mortality rates from colorectal cancer have stagnated in the case of women and increased slightly after about 2005 in the case of men.
This recent increase is a cause for some alarm, but its scale should be contextualized before continuing to discuss it. In the same period where incidence increased, the change would be barely visible on a chart including older ages, for whom mortality has steadily improved.
Even reacting to this modest increase with unnecessary alarm, it should be acknowledged that there are reasons to be hopeful about early-onset colorectal cancer. For one, it’s consistently linked to obesity and it’s likely that this link is to some extent a causal one. Other risk factors for early-onset colorectal cancer, such as alcohol consumption and hyperlipidemia are linked to obesity as well. These links complicate figuring out what exactly the contributions of each of the known factors are to the overall rise. However, their contributions alongside other factors like metabolic syndrome, ulcerative colitis, chronic kidney disease, and so on, at least seem to be large, and thankfully, they are now virtually all indirectly or directly addressable through pharmacotherapy and surgery.
For example, hyperlipidemia is now able to be safely addressed with statins, ezetimibe, and PCSK9 inhibitors. This can be done without problem from a young age. But genetic evidence suggests it will not help us in our quest to address early-onset cancers. That genetic evidence shows that cholesterol levels do not contribute to the risk of the broad category of all cancers. If this holds for colorectal cancer specifically, then that provides public health authorities with information they can use to ‘look elsewhere’ and provide advice that’s likely to help rather than waste.
But obesity does play a causal role in early-onset colorectal cancers and many other ones, and we have an effective treatment for obesity now. The effect sizes found in large-sample and meta-analytic studies of the relationship between GLP-1RA usage and colorectal cancer—among other simultaneously benefitted cancers—suggest that using them at scale would not only halt the rise in early-onset colorectal cancer, but reverse it to a major degree. Because this is easy and can be inexpensive to pursue if the Congress or the current White House, say, negotiate down GLP-1RA prices or buys the patent for generic manufacturers, it should be pursued as a first-line response to the rise in early-onset colorectal cancer.
If, after obesity is reduced as much as we can get it with pharmacotherapeutics, we find that early-onset colorectal cancer incidence rises again, it may then be time to focus on other major risk factors likely to be causally involved, like alcohol consumption. The reason to do this to a lesser degree or possibly after the a weight loss-focused main approach is that this will be far less effective and lives are on the line. Governments can simultaneously pursue multiple lines of action, but in health policy, pursuing one option tends to come at the cost of will that can be applied to pursuing other, potentially more effective ones. Moreover, the government simply has limited ability to reduce alcohol intake, and their ability to find and act on other potential causes—given that other age groups who are equally exposed to the modern environment are doing fine—will, in many cases, be even more limited.
In short, early-onset colorectal cancer incidence and mortality is up, but it’s not up so much that people should be stressing out about it and it does not overturn concerns about overdiagnosis and resulting overtreatment or the generally fortunate trends for other cancers. More importantly, there is a readily-available fix available to reverse this unfortunate trend.
Colorectal Cancer: Why Not An Information Campaign?
A major contributing factor to the risk of death from early-onset colorectal cancer is underdiagnosis.
Early-onset colorectal cancer is underdiagnosed in the sense that, when it’s caught, it usually already become highly-developed: most young patients are only identified as having colorectal cancer in stages three or four. Moreover, young people usually report having multiple symptoms before they’re diagnosed, with a majority mentioning that after identifying that they had serious symptoms, they adopted a ‘wait-and-see’ attitude before pursuing medical care.
To make the situation with early-onset colorectal cancer identification worse, it’s so unusual to get it at a young age, that doctors frequently put up roadblocks for patients. Doctors prefer to focus on more likely and less severe alternative diagnoses to explain their symptoms, and large numbers of doctors will refuse to refer young patients for colonoscopies, let alone do so in a timely manner.
These facts provide clear support for information campaigns. With the rise in incidence, young people ought to know the signs so that when they show up, they don’t drag their feet on pursuing medical care, and they act more forcefully to push their providers to screen them. The more costly possibility is lowering the standard age at which screenings begin and advancing the use of less invasive screenings like fecal occult blood tests and sigmoidoscopies.
Without any effort to engage in a formal cost-benefit analysis, I suspect that informational campaigning would yield more favorable returns than greatly expanding screening. While the latter may lead to more cases identified and lives saved, it’s tremendously more expensive for a condition that is still very rare in the age groups being discussed.
Quick Question and Answer
Is there an early-onset cancer epidemic?
When an epidemic is defined by a large absolute increase in early-onset cancers, the big picture answer is “no”.
But are more young people diagnosed with cancers than they used to be?
Incidence trends are mostly flat or slightly increasing, with notable increases still being limited in number and scale. Broadly-speaking, diagnostic trends are driven more by changes in identification and diagnostic practice than they are by genuine increases in incidence at a given severity level, and an increase in obesity-related cancers has eclipsed any increase in non-obesity-related cancers.
Are more young people being crippled by cancer than before?
No, age-specific DALYs are down, and this is true for the young as well as the old. However, due to increasing rates of overdiagnosis, more young people are being harmed by having their cancers identified.
Are more young people being killed by cancer than before?
No, age-specific death rates are down, and this is true for the young as well as the old.
What’s up with early-onset colorectal cancer incidence?
Colorectal cancer is almost the only major cancer to seriously buck the pleasant trend seen for most other cancers afflicting the young. The explanation for its rise is partly obesity, which we can now address cheaply and efficient, and so we should now do that. The scale of and source for the residual component of the rise is unclear, but it is notable that it has not been credibly linked to any known toxicants.
What’s up with the early-onset colorectal cancer mortality trends?
The answer to this question ought to be largely that it is a natural outgrowth of heightened incidence. More practically, the rise has a lot to do with slow updates to potentially outdated standards of care.
The health system has failed to move rapidly to update towards giving colorectal cancer-related advice to the young and towards giving providers the advice to enhance screening levels for the young. As such, when colorectal cancer is detected among young people, it is generally far more severe than it should have been had people been more careful and acknowledged their symptoms when they occurred. These cancers are also more severe than they would have been compared to the world in which providers are more willing to perform colonoscopies or engage in other diagnostic and preventative procedures with young patients.
Because of the still absolutely low rates of colorectal cancers in the young, the debatable efficacy of available screening methods, and the high cost of said screenings, it is not clear whether expanding the standard of care to encourage screening at lower ages would pass muster in a formal cost-benefit analysis.
For reference, the obesity-related cancers were esophageal, stomach, colorectal, liver, gallbladder and extrahepatic bile duct, pancreatic, corpus uterine, ovarian, kidney, thyroid, and multiple myeloma, whereas the non-obesity-related cancers were lip, oral cavity and pharynx, larynx, lung, melanoma of skin, Kaposi sarcoma, breast, cervix uterine, prostate, testis, bladder, brain and central nervous system, Hodgkin lymphoma, non-Hodgkin lymphoma, and leukemia.
Early-onset breast cancer was classified as non-obesity-related despite postmenopausal breast cancer being obesity-related because the sample was defined to be young enough that menopause was uncommon, and thus the cancers would’ve been premenopausal in large part. Premenopausal breast cancer is negatively correlated with BMI.
This suggests diagnosis may be causing increasingly large amounts of harm, because the prescribed treatments and biopsies are worse than the affliction in the growing share of benign-but-treated-anyway cases.








Another factor is people more willing to talk openly about cancer. I'm just old enough (52) to remember as a small child my grandparents talking with friends. Occasionally a member of the group would say "heard about so-and-so"? This would then be accompanied by muttering about "yes, that's horrible", but the conversation about their illness was always low-voiced. I now know it's because the person had cancer, and they were worried if they said it out loud, someone else would get it.
I'm confused about the scenario where a child has a brain tumor better left undiagnosed. Is the idea that it was harmless?