There Are No More Excuses To Be Fat
We can inject away obesity, even for people with serious genetic predispositions
This was a timed post. The way these work is that if it takes me more than two hours to complete the post, an applet that I made deletes everything I’ve written so far and I abandon the post. You can find my previous timed post here. If you’re looking to acquire Semaglutide, Tirzepatide, Retatrutide or other GLP-1RA drugs at an extremely low price of around $15-$40 per month, see this article.
You really have to hand it to GLP-1 receptor agonists (GLP-1RAs) like Ozempic/Wegovy (semaglutide) and Mounjaro/Zepbound (tirzepatide): they have taken away every last excuse to be fat.
We live in a fat society and no one wants to be fat, so naturally, excuses to be fat are everywhere. These range from ‘I’ll start dieting on Monday’ to ‘I never have the time’ to ‘my genes made me do it’ and the often-wrong ‘But I have hypothyroidism!’ Now that people can inject an effective appetite suppressant, all of that has been shown to be wrong. These excuses are so bad that I’ve decided to go through some of them.
MC4R Mutations
Mutations in the melanocortin 4 receptor (MC4R) gene are purported to be the most common genetic cause of obesity. Individuals expressing a deficient genotype are remarkably hungrier, less likely to be satiated after eating a certain amount, and they have less healthy food preferences.1 The prevalence of pathogenic MC4R variants is clearly elevated in obese populations, as noted in a recent trial re-analysis, they’re found in: “0.3% of an unselected UK birth cohort, 1% of adults with a BMI >30 kg m−2, 2% of children with obesity and up to 5% of children with severe obesity.”
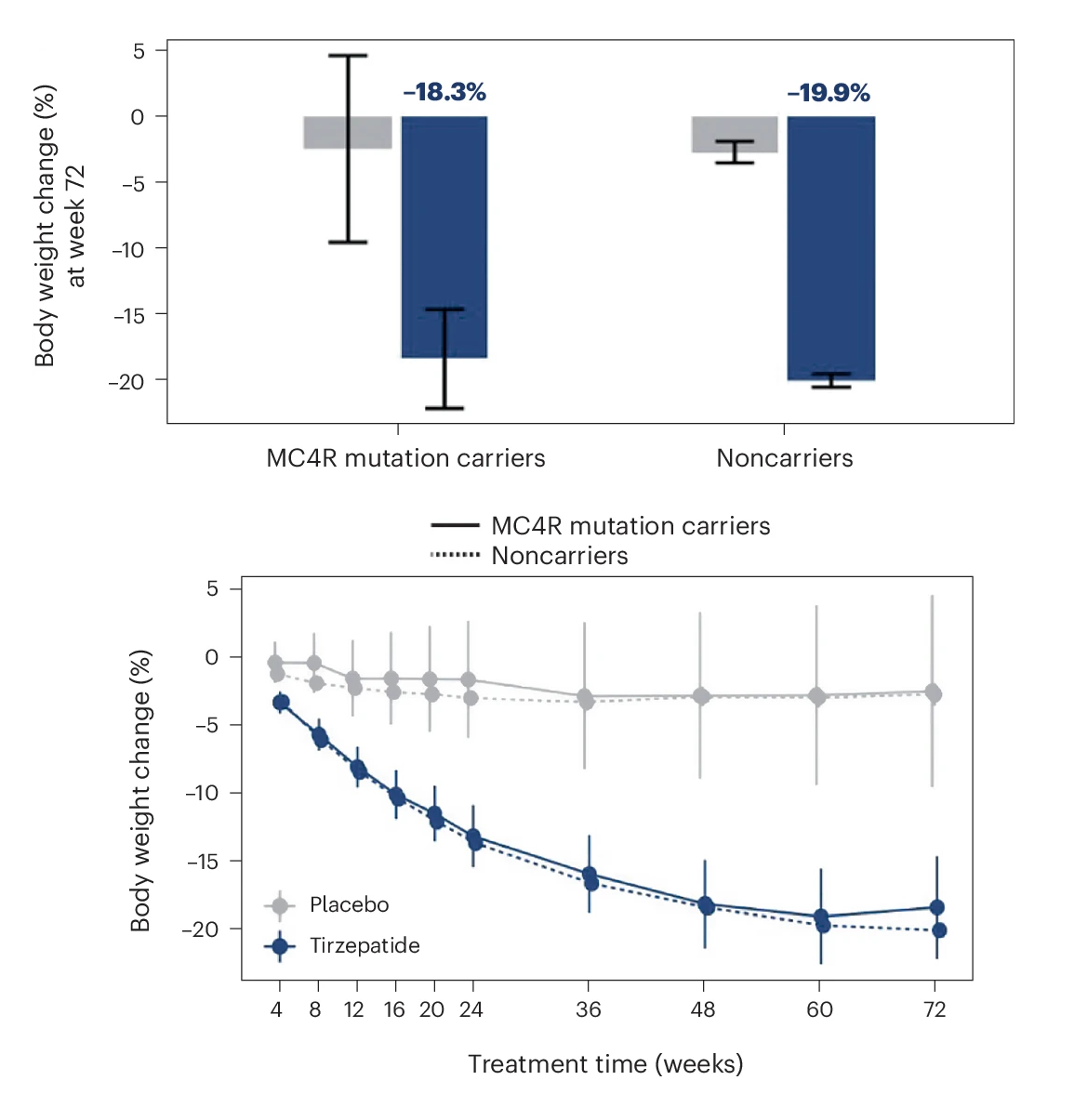
That re-analysis also showed that, though MC4R carriers were somewhat more obese than the other obese people in the SURMOUNT-1 trial, they still got the same benefits from using tirzepatide that ‘normal’ obese people did: there was no effect moderation by carrier status.
In other words, a rare genetic cause of obesity was totally, crushingly defeated by a drug that operates through reducing calories in without affecting calories out beyond what’s expect from weight loss.2 On its own this is a very meaningful finding, but we can go further.3
Common Genetic Causes of Obesity
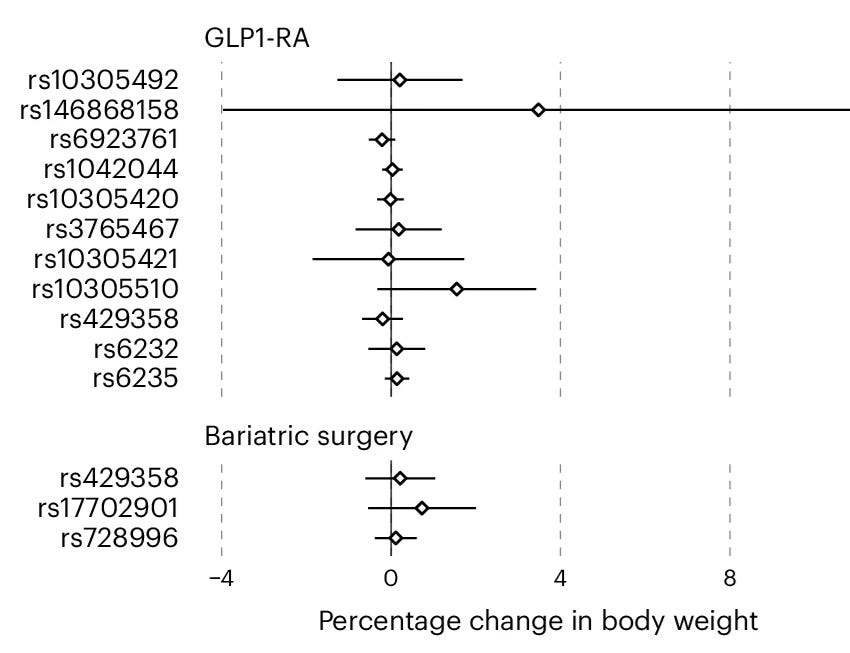
BMI polygenic scores (PGS) predict being fat using common variants. Just as MC4R carrier status fails to moderate GLP-1RA efficacy, these too do not seem to affect how well GLP-1RAs work. In a major cross-sectional study of several biobank samples, researchers documented no apparent moderation of GLP-1RA efficacy by the BMI PGS.4 The same is not true for the effects of bariatric surgery.5
What about rather than using PGS, we leverage known large-effect variants in the gene GLP1R? These can be useful as instruments to understand the long-term effects of GLP-1 receptor agonism, much like the situation with variation in HMGCR. The authors showed that result alongside results for variants in ApoE, PCSK1, and PKHD1. The result was the same as the result for the BMI PGS: nothing.
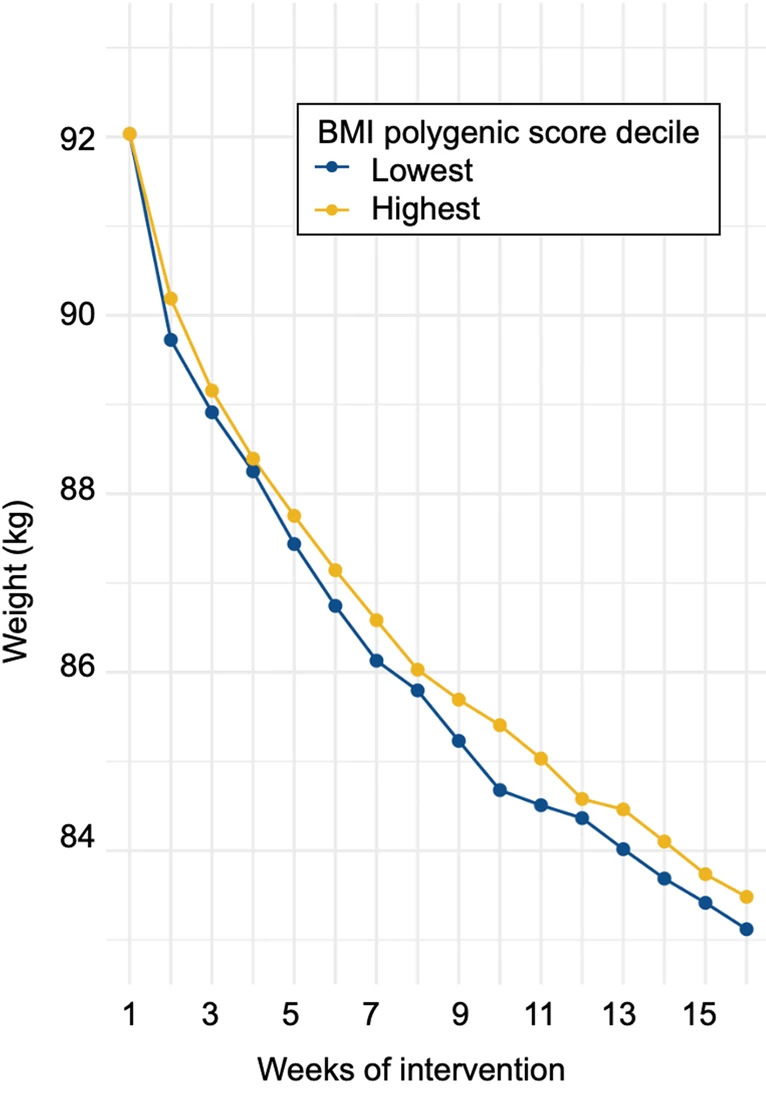
These results do not imply that BMI PGS are not moderators of success at attempted weight loss. They are! Consider this result from the Spanish ONTIME study, where individuals with higher BMI PGS (and thus greater predicted BMI) dropped weight more slowly:
The same article replicated this finding for various variants implicated in obesity and weight loss using data from different studies conducted across Europe and in Canada.
The distinction between the results of these papers is important. Natural variation in several genes including GLP1R modifies how easy it is for a person to gain or lose weight, but practically anyone who injects a GLP-1RA will lose weight, regardless of their genes, up to and including genes whose effects involve impaired GLP1R in currently known ways. GLP-1RAs are effectively an equalizer for people with different obesity genotypes!6
Hypothyroidism
I’ve known far too many people who have told me their obesity is due to hypothyroidism. Hypothyroidism only has a small effect on total metabolism, so people’s statements about its immense power to stack on the pounds are unrealistic, but I digress. We do know that GLP-1RAs work for people with hypothyroidism.
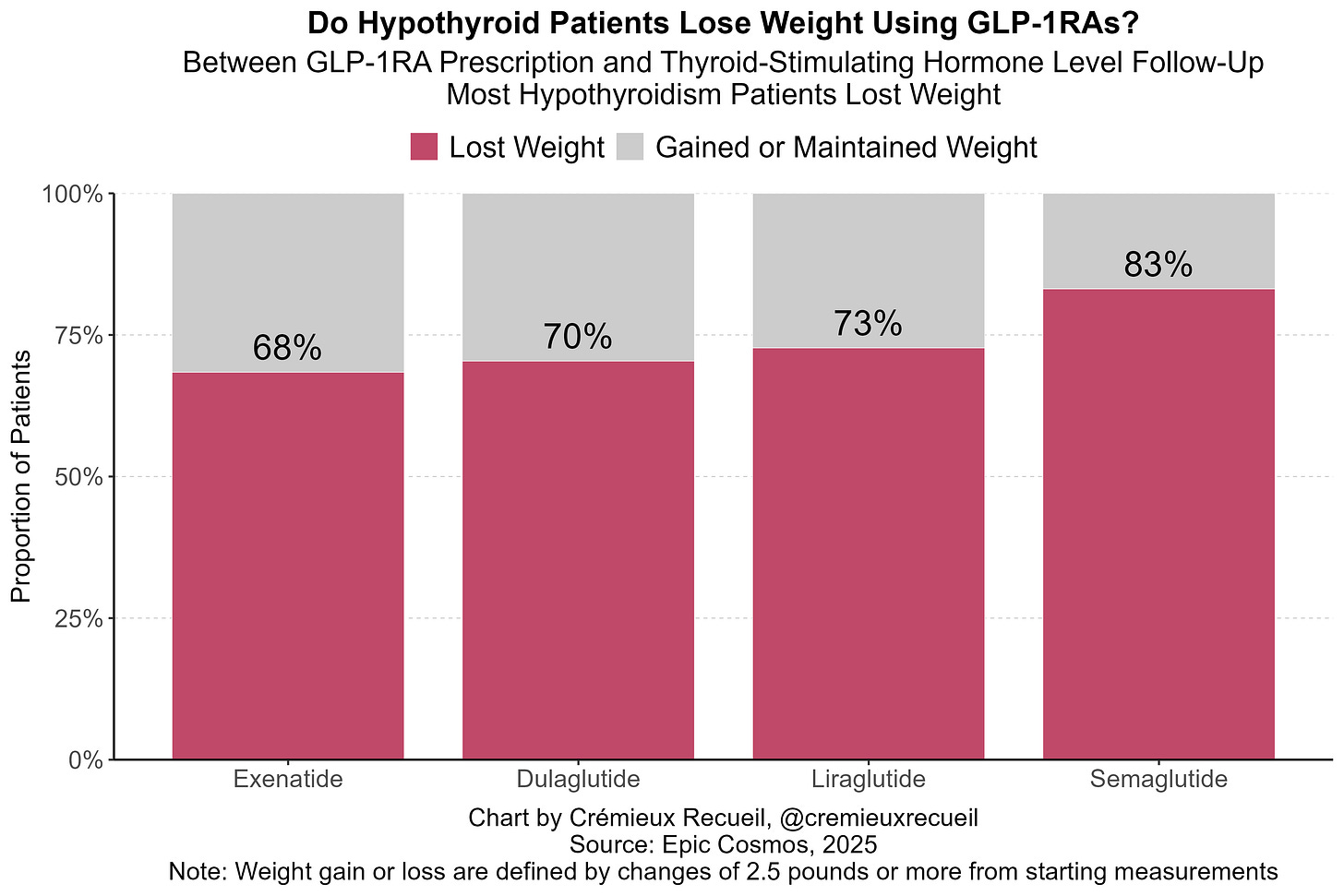
Using all available data in the Epic Cosmos dataset, we can see that most hypothyroidism patients do achieve weight loss, even in the short timeframe I’ve been forced to use for reasons of statistical power:
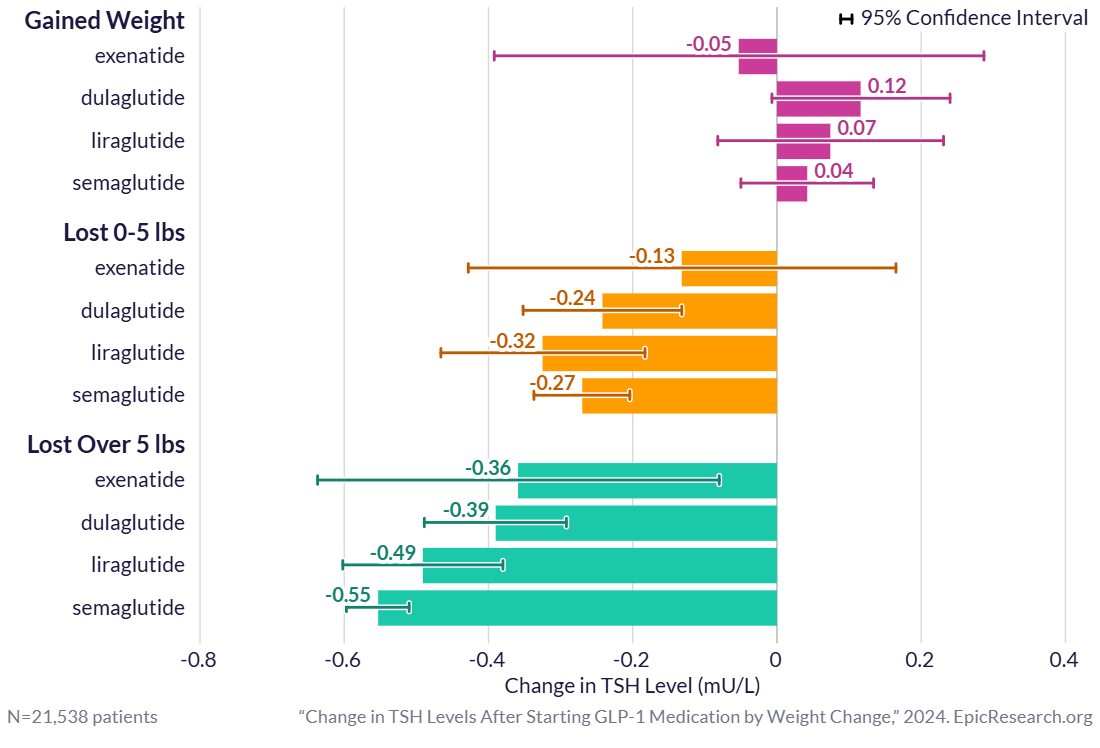
Furthermore, after matching on starting weight, age, sex, race, dosage for interval, GLP-1RA, and HbA1C, there is no statistically or clinically significant difference in rates of weight loss over the same time periods (up to two years) for individuals with or without a diagnosis of hypothyroidism (E03.9). Beyond this finding, others have shown that, not only do GLP-1RAs induce weight loss among those with hypothyroidism, they also measurably improve thyroid-stimulating hormone levels, alleviating hypothyroidism!
The finding of hypothyroidism improvement has replicated with exenatide and liraglutide, and has worked out so strongly it necessitated thyroid medication updates in two case studies involving semaglutide. With this background, it’s important to note that there is no meaningful cohort-level evidence for a GLP-1RA association with thyroid cancer, nor does the trial-based evidence support concerns.
Hypothalamic Obesity
The hypothalamus manages temperature, hunger, thirst, libido, sleep, weight, reward, and more. Damage to it can cause a severe form of obesity dubbed hypothalamic obesity. In the past, this was a very good excuse for someone to be fat. After all, issues with a person’s reward system could really mess them up. But now, it appears that even this very serious, rare cause of obesity is no longer a valid excuse.
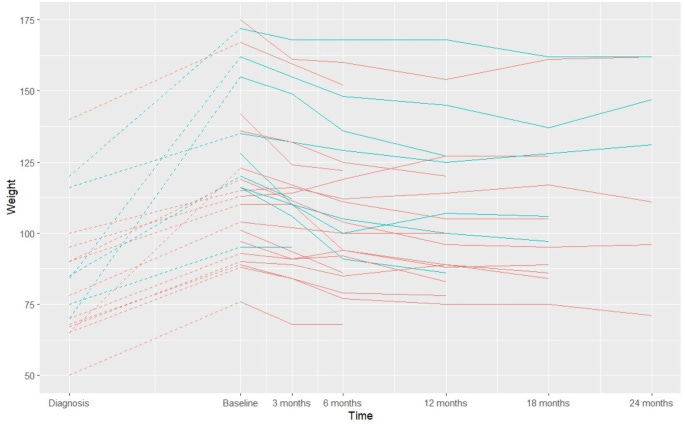
A case study in four women with hypothalamic obesity due to craniopharyngioma (a rare, non-cancerous brain tumor) saw them losing an average 17% of their body weight over six months using semaglutide. They safely maintained about this level over two years.
In another sample, this time of 26 patients, initial diagnosis with hypothalamic damage was accompanied by a median BMI of 25. After diagnosis, patient BMIs quickly rose to a staggering median of 38 when they started taking semaglutide. Over a period of up to two years following treatment initiation, patients dramatically reduced their BMIs. At one year, they averaged a 4.4-point BMI reduction.
This has significantly replicated with exenatide, in addition to only directionally replicating in a study that was likely too small. I’m not too shocked by that result only being directional; as I’ve remarked before, exenatide is weak. Nevertheless, all case studies and trials for hypothalamic obesity agree.
Schizophrenia
Schizophrenics have a higher obesity rate than the general population. For many patients, it is unfortunately something that defines their lives and that they seem to always struggle with. A recent study voiced this concern and showed that once-weekly semaglutide helped even schizophrenics to safely drop weight and keep it off.
A more worrying fact about schizophrenics and weight is that the medications that help many of them to stay at least somewhat sane also cause them to become fat. Clozapine, for example, is the most effective antipsychotic for persons with treatment-resistant schizophrenia. Large numbers of schizophrenics are forced by circumstance to take drugs like clozapine lest they risk a psychotic episode, effectively forcing them to choose obesity in the process.
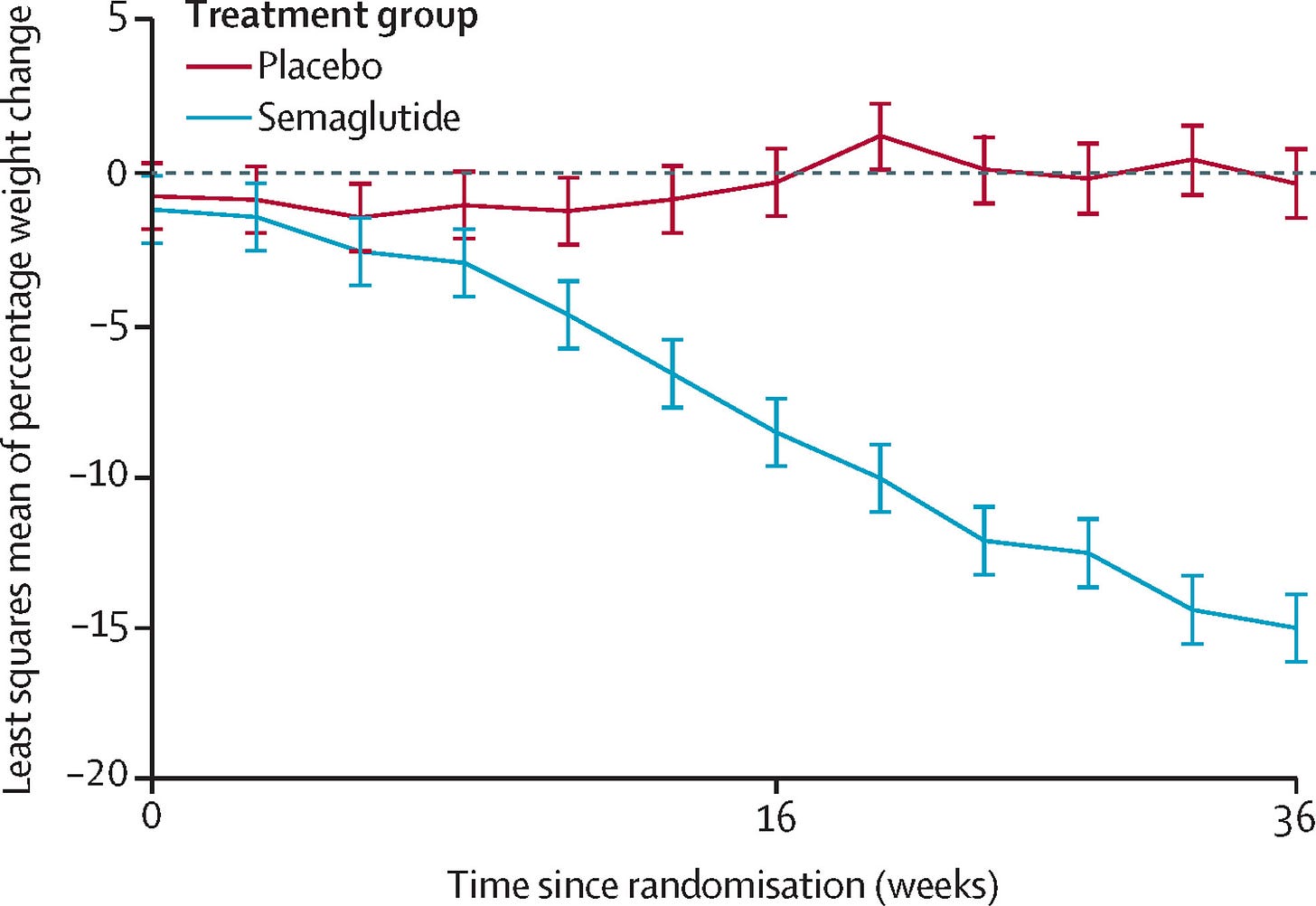
The Australian COaST phase-2 trial randomized schizophrenics who were taking clozapine to either receive a placebo or semaglutide. The result was about what you’d expect if you’re familiar with the literature on GLP-1RAs and exactly what you’d expect if you’ve read this article up to this point: people lost weight.
The weight loss schizophrenics can experience with GLP-1RAs is important in its own right, but it’s not going to be worth much if it interferes with their medication and makes them less sane. This is a real worry given that these drugs can cause (generally temporary) delayed gastric emptying (gastroparesis). Luckily, the investigators looked into that and found no apparent worsening of psychotic symptoms and no lowering of clozapine concentrations. Success!
This finding has replicated in a trial of liraglutide7 and in another trial of semaglutide. [December 4, 2025: this replicated once again in a trial of semaglutide.]
Grab Bag
By now, we’ve hit the high notes. Things that cause serious weight gain and make people feel like their lives are out of control are roundly beaten with GLP-1RAs, so now I’m going to point at some rare things we have some evidence GLP-1RAs can assist with or conquer.
ROHHAD stands for rapid-onset obesity with hypothalamic dysfunction, and it’s an ultra-rare condition that causes severe weight gain. In what I believe to be the only available case study, semaglutide appeared to work in a French female sufferer from this condition.
Prader-Willi syndrome is a disorder caused by issues with chromosome 15. It’s characterized by poor muscular tone, stunting and developmental delay, and relentless hunger leading to hyperphagia, or excessive overeating.8 The result is that Prader-Willi sufferers become extremely fat. In one case study, liraglutide ended the hyperphagia and led to weight loss. After release from the hospital, the patient also unprecedentedly maintained their weight for a year. A trial of liraglutide in young child sufferers returned unimpressive results that were not statistically significant, but it’s unclear how much age matters in this condition. The trial did, however, show liraglutide helping with hyperphagia. In a case series of three Prader-Willi sufferers, one patient stopped gaining weight and the other two managed to considerably reduce their weight using semaglutide.
Bardet-Biedl syndrome is a peculiar and extremely rare genetic ciliopathy, meaning a disorder of the cellular cilia. The condition comes with a hodge-podge of symptoms ranging from visual problems, to extra fingers and toes, excessive thirst and hunger, diabetes, an inability to smell, hypogonadism, mental retardation, deafness, spastic movement, impaired renal function, obesity, and more. In preclinical data, semaglutide seems to help with the overeating part of this condition. This held up in at least one human case study.
Alström syndrome is a rare autosomal recessive genetic disorder characterized by blindness, hearing loss, heart issues, type-2 diabetes, short stature, and obesity. In a sample of 72 British adults with this condition, GLP-1RAs successfully reduced patient weight.
A case study of two patients with 16p11.2 deletion syndrome—which causes mental retardation and obesity—and two patients harboring pathogenic MC4R variants showed considerable weight loss with liraglutide. The same treatment seemed to reduce weight in a sample of 23 adults with molecularly-confirmed genetic obesity from various sources. The same study saw improvements with naltrexone-bupropion as well.
Cushing’s syndrome is ‘moon face’, thin limbs, easy bruising, high blood pressure and out of control glycemia along with obesity caused by excessive adrenal production of cortisol. A 275-pound female patient with this condition titrated up from 0.25 to 1mg per week of semaglutide and managed to lose 42 pounds in the process before stalling out. The patient was then prescribed levoketoconazole for cortisol control and they managed to lose an additional 47 pounds for a total weight loss of 89 pounds.
Increasingly many monogenic obesity syndromes and conditions that cause obesity are being treated to varying degrees with GLP-1RAs. The list can go on because this is a hot fad that I’m hopeful does not end any time soon, since it offers a real opportunity to improve lives and to show us just how far we can go improving obesity for even the most traditionally dismal, seemingly hopeless, and neglected cases.
No Excuses
The only rigorously confirmed non-dosage moderators of GLP-1RA weight loss efficacy are as follows:
Sex
Diabetes and baseline glycemia
The constellation of initial BMI/adiposity/obesity/etc.
Discontinuation9
For almost everyone, the number of legitimate excuses to be fat has been cut down to:10
Just started the drugs
Preexisting conditions precluding use
Fear of needles
Cost
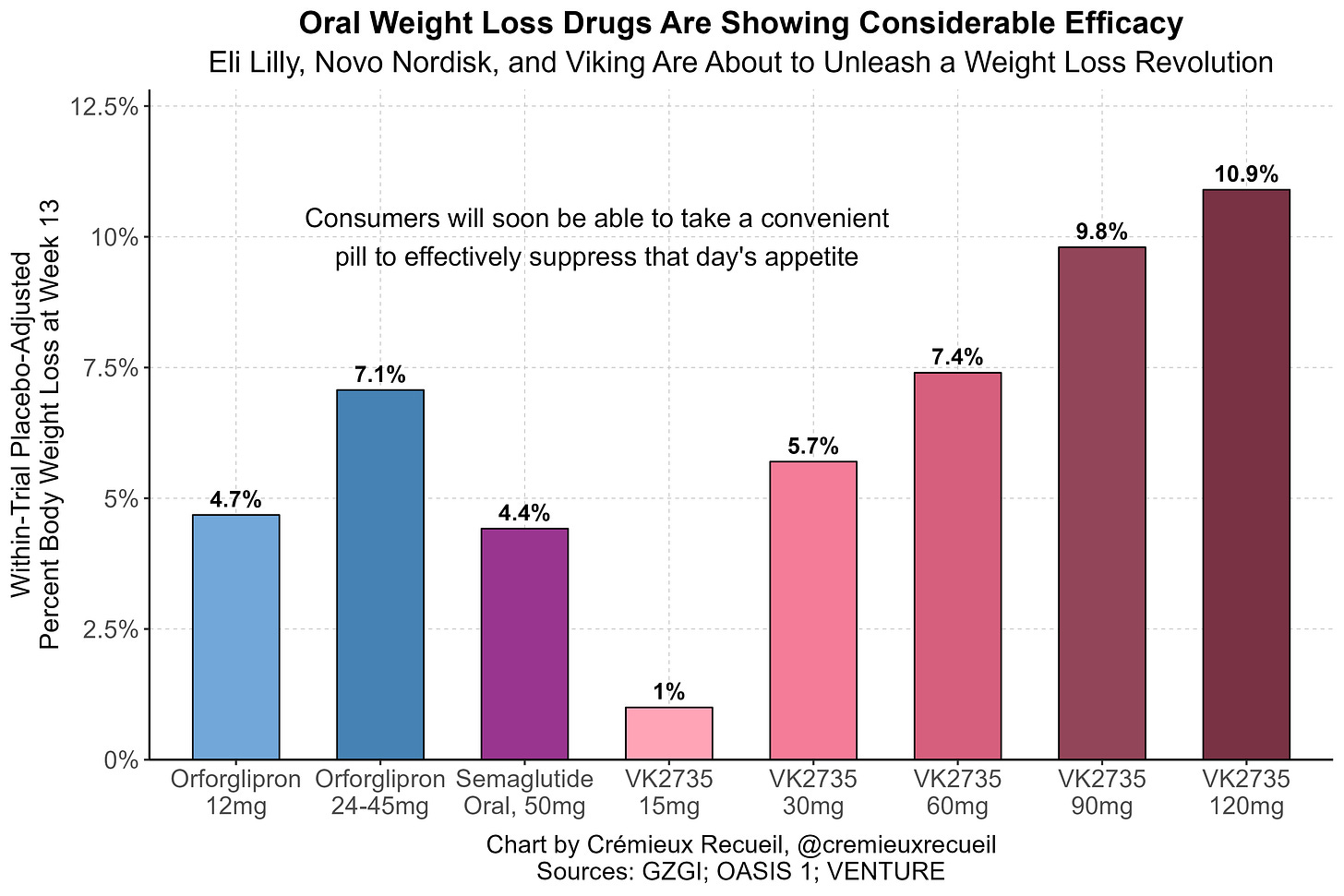
The most common barriers that remain are fear of needles and cost. For needles, we have good news: convenient and effective GLP-1RA pills are about to hit the market!
When it comes to cost, the good news is that prices are falling all the time, and as more competition enters the market, net prices will no doubt continue their descent. The even better news is that, for the time being, anyone cost-constrained and sufficiently motivated can take advantage of the very low prices on the gray market!
It’ll no doubt be a few years before most people realize it, but it’s true: there really are no excuses to be fat anymore. It’s a good thing that every excuse is meeting the same fate. That fact means that, soon enough, nobody will have to be fat.
November 3rd 2025 Update: Menopause
I’ve had so many older women ask me if these drugs will help them to lose weight after hitting menopause. Very large numbers of women hit menopause and then find it practically impossible to cut weight anymore, which is extremely understandable. Just think about what menopause is! The analogy I give to men is that menopause is essentially like reaching a point in life where your testicles fall off. It’s like a one-off event that ages women radically overnight.
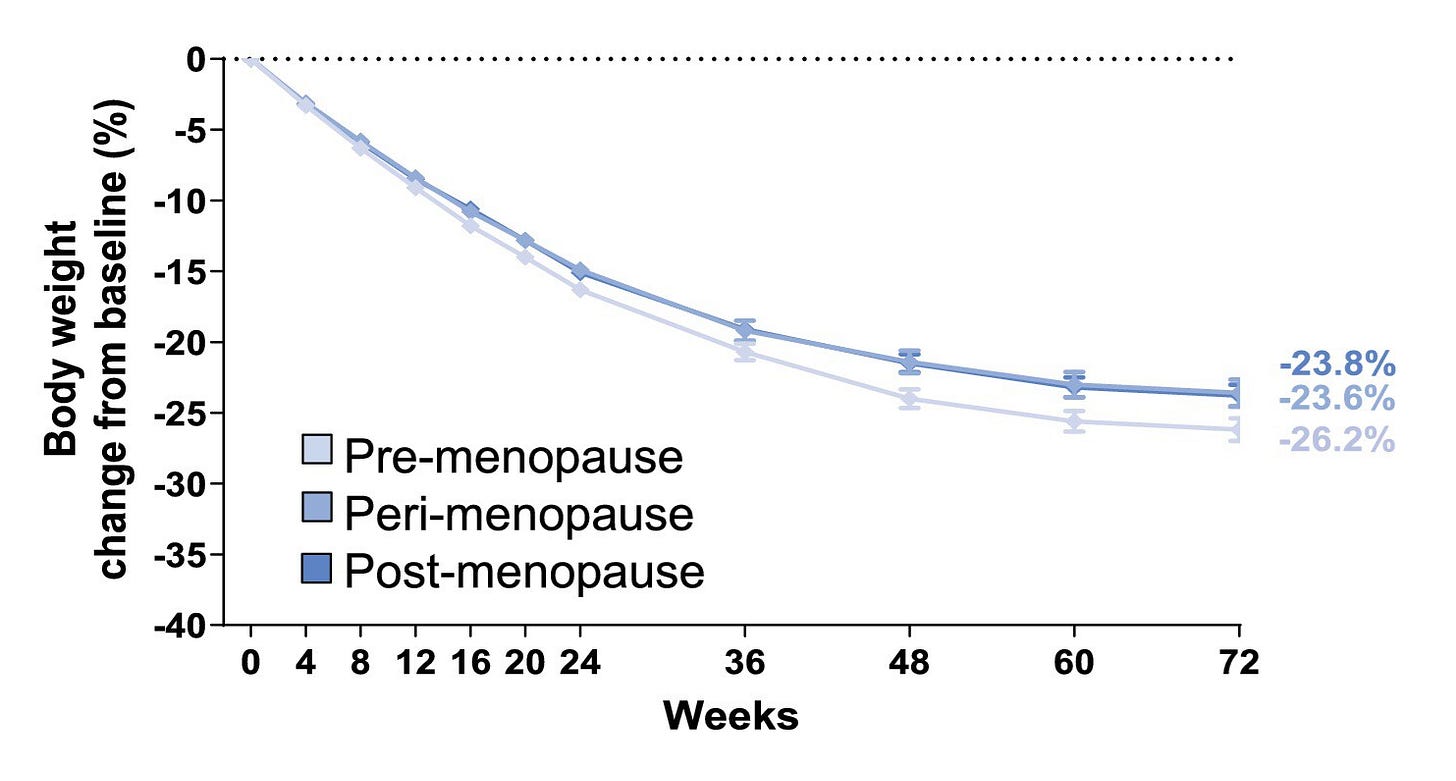
As it turns out, we do have data on this very topic. If you’ve read the rest of this article, you probably know what the result is already: menopausal women lose weight with GLP-1RAs just as easily as pre- and perimenopausal women. Take a look at this result from the 72-week SURMOUNT-1 trial:
There is a slight difference, but it’s not clinically meaningful, and if I had to guess, it’s better explained by age-related covariates like diabetes status. The main thing to notice is that the results are practically the same by menopause status. [November 4, 2025: The author of this research noted that this result replicates.]
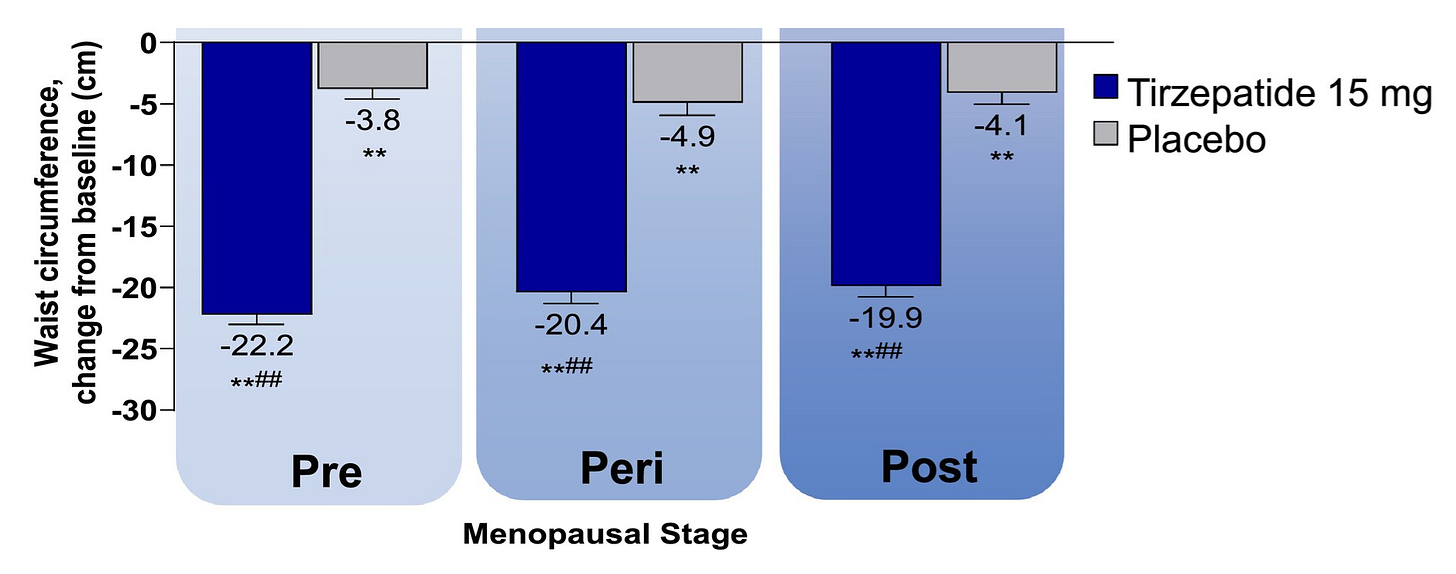
Another worry about weight loss after menopause is that it won’t be as feminine (meaning as well targeted to be around the waist rather than the breast and buttocks) as weight loss prior to menopause. Rest assured, that is not a realistic concern. You lose fat where your fat is, so how you lost weight before menopause will likely be how you lost weight after. But to add some assurance, look at the waist circumference declines across these groups. They were highly similar:
So to reiterate the post’s major point… there are no excuses to be fat anymore!
November 14th 2025 Update: PCOS
Polycystic ovary syndrome (PCOS) sufferers often report that they have trouble dieting and losing weight, and consistent with that notion, the condition has been associated with obesity, type-2 diabetes, and insulin resistance. But, nevertheless, in real-world data, PCOS sufferers still manage to lose weight using GLP-1RAs. In electronic health record data, PCOS patients who start dulaglutide, exenatide, liraglutide, semaglutide, or tirzepatide show significant weight loss after a year of usage:
PCOS patients also show marked reductions in HbA1c, indicating they they’re less likely to be diabetic or prediabetic after getting on these drugs. If we had data available for them, I’d also wager that their insulin resistance improves, like it does for other GLP-1RA users.
The scale of these improvements is similar to the scale of improvements for other groups observed in EHR data. Even if the extent was less, we could still confidently say: every excuse for being fat that we have data for is still getting shot down!
February 18th 2026 Update: Old Age
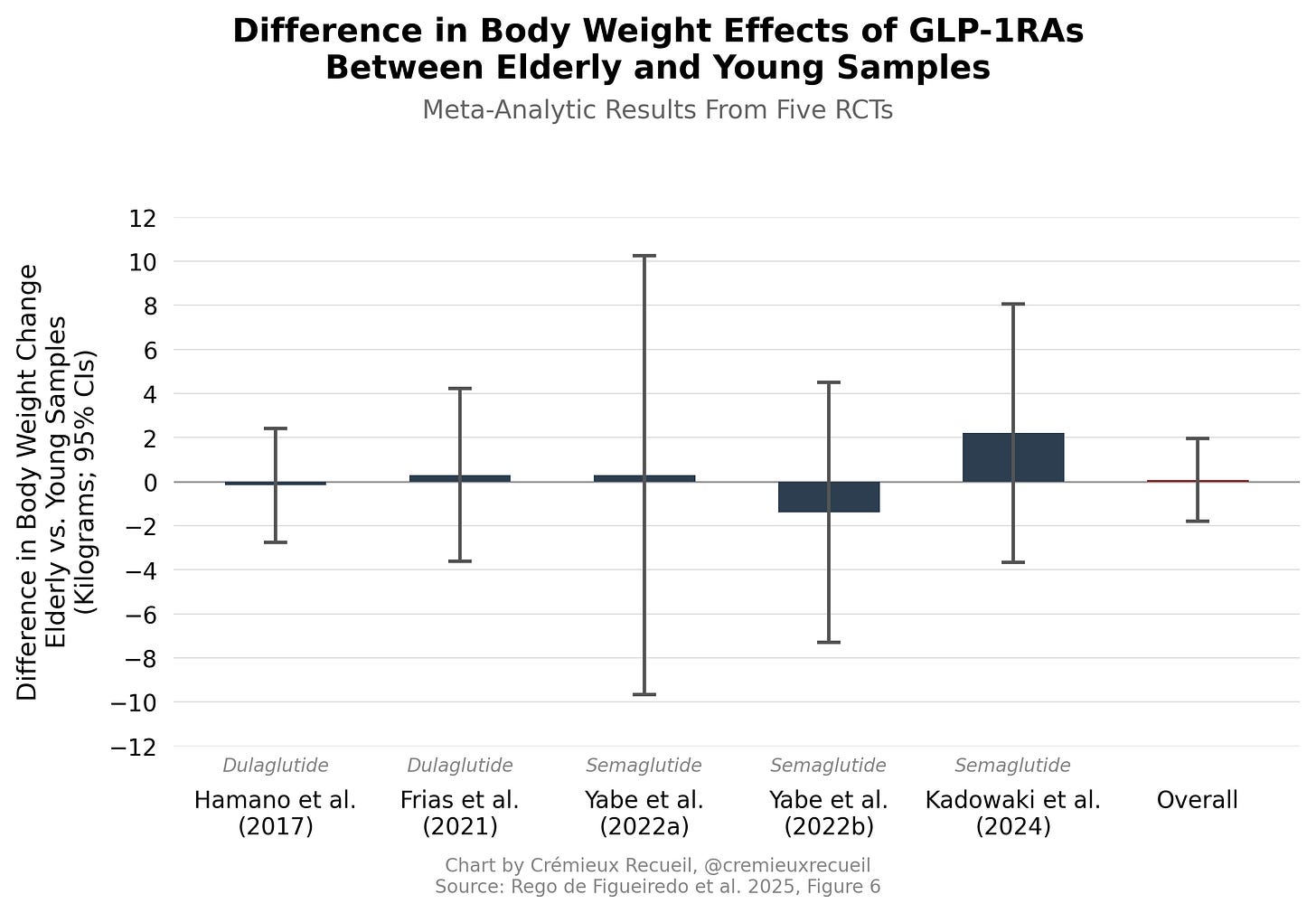
A new meta-analysis has come out on the topic of whether GLP-1RAs work equivalently for elderly and young persons. The results were straightforward and predictable if you’ve read the rest of this article.
Across up to five randomized, controlled trials which involved either dulaglutide (2) or semaglutide (3), the elderly and younger samples had indistinguishable rates of serious adverse events, they had similar rates of nausea, vomiting, and diarrhea, and the old had a (d ≈ 0.40) higher risk of constipation (p = 0.025 before multiple comparisons correction), which is something they were at a greater risk of anyway. The old also had a significantly higher risk of hypoglycemia (d ≈ 0.54), which is predictable given that old people tend to have less muscle, worse diets, etc. All of these differences were either too meager to matter or modest and manageable.
When it came to efficacy, the age difference for HbA1c effects was nonsignificant and not clinically meaningful, despite the hypoglycemia result. The more interesting efficacy result was for weight loss, where the difference was null (p = 0.90). Or, in other words, GLP-1RAs seem to lead to equivalent weight loss for both young and old.
Though the study is not about MC4R carriers specifically, there is evidence that tirzepatide treatment improves food preferences.
Based on the popular notion that GLP-1RAs cause excess lean mass loss, you might expect otherwise. But that popular notion is not empirically-supported.
It should be noted that this systematic trial-based evidence was preempted by a case study with liraglutide and a small trial that also used liraglutide.
The type-2 diabetes null finding may seem odd in light of the well-documented moderating influence of type-2 diabetes on rates of weight loss and GLP-1RA efficacy. The samples used in this study were at least 48% diabetics and diabetes status was not a significant moderator in their models including genetic risk. I suspect that what we’re seeing here is that the score is not the trait, even if it clearly is correlated with it, with inflated standard errors being the result.
Nevertheless, this isn’t relevant, as the point is to note genetic excuses are not clinically or statistically significant moderators of GLP-1RA efficacy, and so long as we are using what people consider to be an excuse (i.e., any reasonably valid PGS), we’re alright for that inference.
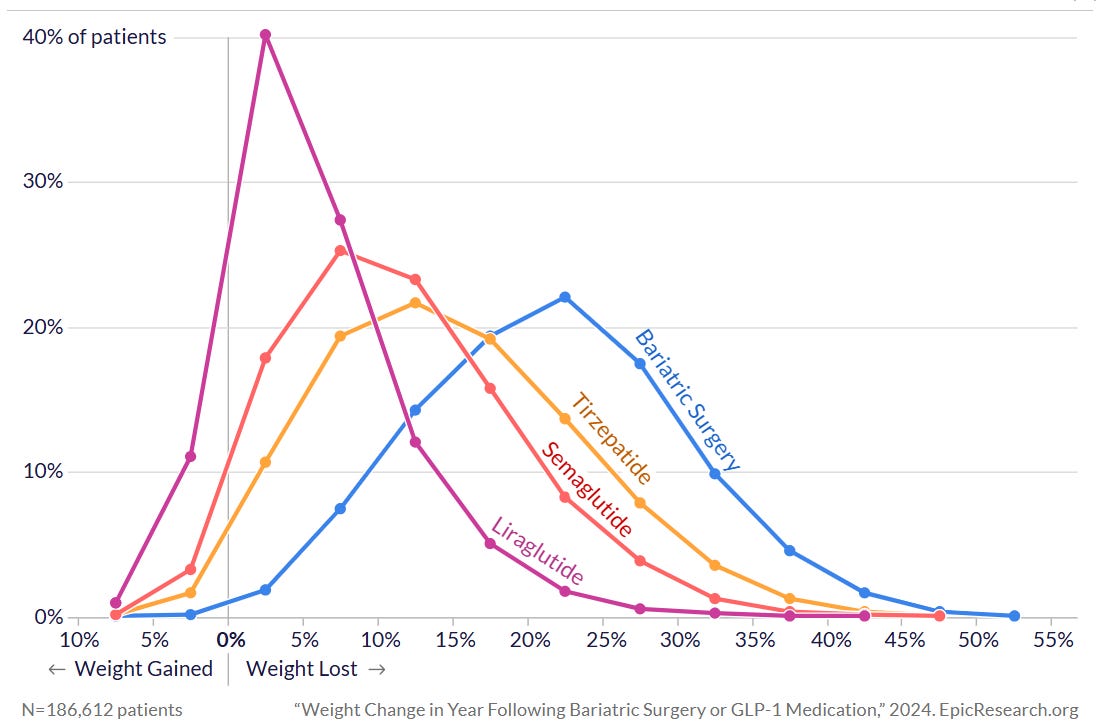
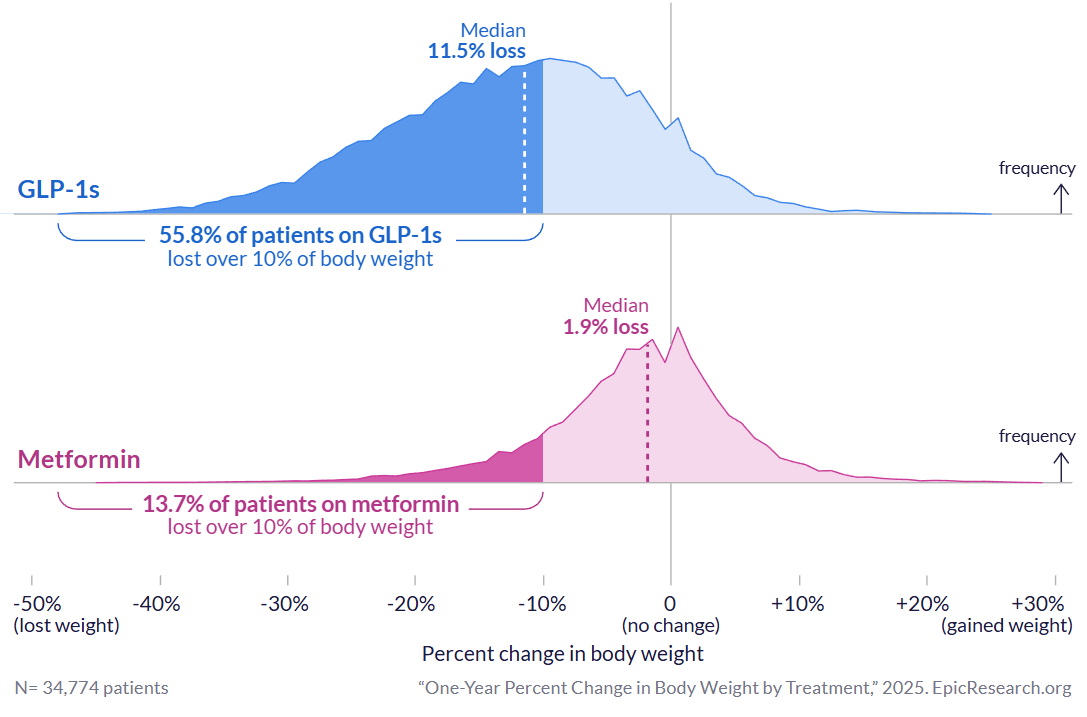
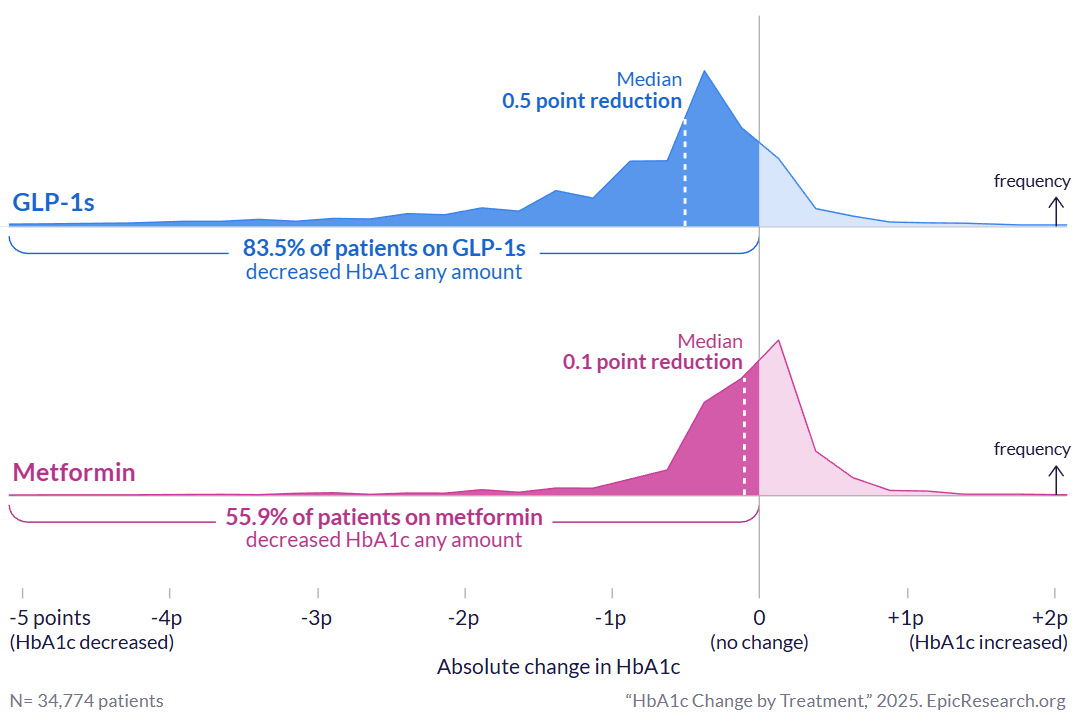
This chart shows cross-sectional results that are less optimistic than the results from trials. The reasons for the discrepancy have to do with factors like discontinuation, differences in dosing, disuse of prescriptions, patient heterogeneity, and so on—standard real-world qualifiers of drug efficacy. Moreover, this chart is missing results for the third-generation GLP-1RA retatrutide, which is even more effective for generating weight loss than either tirzepatide or semaglutide.
Going by the standard definition of successful weight loss (≥10% weight loss kept off for a year), retatrutide delivers ≥90% success at reaching the weight loss threshold for non-diabetic obese individuals taking an 8mg weekly dose and >70% success for non-diabetic obese individuals on a 4mg dose, by 48 weeks. Both rates would be even higher were individuals prescribed the drugs for longer. Remarkably, even diabetics—who have more trouble losing weight in general, even on GLP-1RAs—managed to reach this lofty weight loss target 24% of the time by 40 weeks using a 1mg dose of semaglutide and 57% of the time using a 15mg dose of tirzepatide in the SURPASS-2 trial. Other trials reach similar conclusions (e.g., high efficacy for all modern GLP-1RAs; superior efficacy for tirzepatide than for semaglutide; inferior efficacy for diabetics than for non-diabetics).
The authors behind that trial have also commented on the risk of anhedonia and blunted affect. That’s worth a read if you’re interested in that topic.
Notably, just as papers have reported MC4R mutations are the most common genetic cause of obesity, so too have papers on Prader-Willi syndrome. The MC4R papers have a stronger case given the frequencies of carrier status versus Prader-Willi syndrome; the Prader-Willi papers have a stronger case on the basis of the much larger effect of the single genetic issue behind Prader-Willi. There’s room—but not a point—for debating who’s right.
You could perhaps throw in the mishmash category of ‘rare side effects that make the drugs intolerable for a small portion of people’ such as binge eating-induced vomiting or gastroparesis and the like, but these would be permutations of discontinuation. In any case, most of these issues are preventable for the majority of people. It’s also not clear that gastrointestinal adverse events moderate weight loss. They did not seem to do so in SUSTAIN 1-5, as only a piddling 0.07-0.5 kilograms of the treatment-placebo difference ended up being explicable by nausea or vomiting.
Of course excluding people like those with hypothalamic obesity and other extremely serious conditions that can be alleviated by GLP-1RAs but, I assume, not fixed entirely after the issue has gotten severe enough. The hope for those, it should be noted, is that eventually these drugs can be given early in obesity development to prevent it entirely. Because of these exceptions, the title of this article is tongue-in-cheek and the footnoted statement must be interpreted with the keyword “almost” considered strongly: there is no excuse for the overwhelming majority of people.




I’ve had this debate a lot of times in a very personal way.
1) until glp-1s, every weight loss claim was snake oil at best and absolutely harmful at worst
2) conscientious people noticed this and reject glp-1s based on this experience
3) I’m personally convinced “this time it different” by the evidence, but it’s going to take at least a generation to get different results.
4) don’t judge people who have good instincts based on all human experience up until five minutes ago. Try to educate them as best you can
Thank you for the info. One common cause of overweight these days is antidepressant use. Weight gain's a common side effect. Dunno whether anyone's figured out whether people on the drugs eat more, or whether there's a metabolic change. Any info on whether these weight loss drugs work just as well when zoloft et al. are the culprit?